From 1 July 2025, the Australian Government is introducing significant changes to the Chronic Disease Management (CDM) Framework. GP Management Plans (GPMPs) and Team Care Arrangements (TCAs) will be replaced with a single GP Chronic Condition Management Plan (GPCCMP). The changes are designed to reduce administrative burden, improve continuity of care, and support better patient outcomes.
Bp Premier is supporting practices through this transition in key stages:
- The July 2025 Data Update will include new MBS items, updates to care plan templates, reminder reasons, and appointment types to support billing and clinical activity under the new Chronic Disease Management (CDM) framework.
- Future Bp Premier program updates will provide additional functionality, including updated co-claiming logic, updated EPC workflows, enhancements to referral workflows, and MyMedicare Medicare Web Services integration.
This article will be updated as additional information becomes available.
In this article:
Overview of the Chronic Condition Management framework
From 1 July 2025, GP Management Plans (GPMPs) and Team Care Arrangements (TCAs) will be replaced with a single GP Chronic Condition Management Plan (GPCCMP). These changes were developed in response to recommendations from the MBS Review Taskforce and are intended to streamline chronic condition management while preserving flexibility for patients and providers.
Key Dates and Transition Timelines
From 1 July 2025, the following MBS item numbers used for GP Management Plans (GPMPs), Team Care Arrangements (TCAs), and reviews will be ceased:
- GPMPs: 229, 721, 92024, 92055
- TCAs: 230, 723, 92025, 92056
- Reviews: 233, 732, 92028, 92059
The ceased item numbers cannot be billed after 30 June 2025 and will be replaced by a new set of item numbers that support the introduction of the GP Chronic Condition Management Plan (GPCCMP).
Practices can continue to manage patients with existing GPMPs or TCAs during a transition period that ends on 30 June 2027.
During this time:
- Existing referral arrangements will remain valid until all services have been provided.
- Individual and group allied health services may continue to be claimed under plans written prior to 1 July 2025.
- Reviews of legacy plans should be transitioned to the new GPCCMP format as of 1 July 2025.
From 1 July 2027, only GPCCMP-based plans will be accepted for access to MBS-funded allied health and related services. Practices will need to ensure that all chronic condition care plans are transitioned before this date.
New MBS Items Available from 1 July 2025
The following MBS item numbers support the preparation and review of the GPCCMP and will be available in Bp Premier from 1 July 2025:
|
|
General Practitioner item numbers |
Prescribed medical practitioner item numbers (non-VR) |
|---|---|---|
New items (from 1 July 2025) |
||
|
Develop a GP chronic condition management plan (GPCCMP) |
Face to Face – 965 |
Face to Face – 392 |
|
Telehealth (Video) – 92029 |
Telehealth (Video) – 92060 |
|
|
Review a GP chronic condition management plan |
Face to Face – 967 |
Face to Face – 393 |
|
Telehealth (Video) - 92030 |
Telehealth (Video) - 92061 |
|
The new items apply to both face-to-face and telehealth services and are designed to reflect updated clinical and administrative requirements.
Billing rules include:
- GPCCMP preparation can be claimed once every 12 months, if clinically appropriate.
- Reviews can be claimed every 3 months, if clinically appropriate.
- To maintain access to MBS-funded Allied Health Services, a GPCCMP must have been prepared or reviewed within the last 18 months.
- To encourage reviews and ongoing care, the MBS fees for planning and review items will be equalised.
- Consistent with current arrangements, items for the preparation or review of a GPCCMP cannot be co-claimed on the same day as general attendance items. Future versions of Bp Premier will support validation for co-claiming rules.
Visit the MBS Online website for more information on the MBS Items for GP Chronic Condition Management Plans.
Practitioner eligibility and team involvement
GPCCMP items may be billed by:
- General Practitioners.
- Prescribed Medical Practitioners.
The following clinical roles will be authorised to assist a GP or prescribed medical practitioner in preparing or reviewing a GPCCMP:
- Practice Nurses
- Aboriginal and Torres Strait Islander Health Practitioners
- Aboriginal Health Workers.
MyMedicare Requirements
For patients registered with MyMedicare:
- To support continuity of care, patients registered through MyMedicare will be required to access GPCCMP services through the practice where they are registered.
- Patients not registered with MyMedicare may continue to access GPCCMP services through their usual GP or practice.
This rule applies to both in-person and telehealth (video) consultations.
Allied Health Referrals
From 1 July 2025, referrals to Allied Health Services can be issued using a standard referral letter and no longer require a structured Medicare form.
To provide patients with greater choice and flexibility. Referrals to allied health services do not need to:
- Specify the name of the allied health provider to provide the services.
- Specify the number of services to be provided.
- Referring medical practitioners can still specify the number of services to be provided under the referral if they choose to do so.
Patients can access care from any eligible allied health provider, regardless of their location or availability.
Key changes from 1 July 2025:
- Referral letters remain valid for up to 18 months, unless otherwise stated.
- Allied health providers must continue to send written reports back to the referring GP following certain services.
- Referrals may be signed and sent electronically.
- Referrals created before 1 July 2025 under GPMP/TCA arrangements remain valid until the allocated services are completed.
Prepare your Practice for GPCCMP changes
With the introduction of the GP Chronic Condition Management Plan (GPCCMP) on 1 July 2025, practices are encouraged to begin preparing in advance.
- Register for your practice for MyMedicare
- Educate and enrol patients for MyMedicare
- Educate staff
- Engage with Primary Health Networks (PHNs)
- Finalise GPMP and TCA billings prior to 1 July 2025
- Check for any care plan appointments that have not yet been billed and complete the billing process.
- Review your held invoices and submit any that include GPMP or TCA items.
- Check your debtors list for items incorrectly billed to patients and reissue these claims to Medicare where appropriate.
- Resolve any online claiming rejections related to GPMP or TCA services and resubmit them for payment before the old item numbers are removed.
- Review and update care plan templates
- Review local address book for Allied Health Contacts
Ensure your practice is registered with MyMedicare to facilitate patient enrolment and compliance with the new requirements.
Inform patients, especially those with chronic conditions, about the benefits of MyMedicare registration and assist them in the enrolment process.
Provide training for GPs, practice nurses, and other relevant staff on the new chronic condition management plan requirements and referral processes.
To support practices in understanding the upcoming changes to the Chronic Disease Management framework, Best Practice Software has developed an eLearning course:
Seek support and resources from your local PHN to assist with the transition to the new system and to participate in any available training or informational sessions.
To locate your local PHN, visit the website of the Department of Health, Disability and Ageing and use the Primary Health Network (PHN) locator tool.
All unbilled GPMP and TCA items must be submitted before 1 July 2025. After this date, these item numbers will no longer be claimable through Medicare. It’s recommended that you:
Custom GPMP and TCA templates will not be automatically updated. If your practice uses custom Word Processor templates for chronic disease management, you will need to manually update them to reflect the new plan structure. This includes removing references to separate team care arrangements and ensuring your templates reflect the new GPCCMP model.
See Create and edit word processor templates for more information.
This is a good opportunity to review and update your contact list for local allied health providers. With the move to referral letters (rather than structured TCA forms), ensuring you have accurate, up-to-date details for relevant providers will help maintain referral pathways.
Check contact names, phone numbers, email addresses, and practice locations in your Bp Premier address book and make any necessary updates.
Bp Premier July 2025 Data Update
To support practices with the changes to the Chronic Disease Management (CDM) framework, the July 2025 Data Update will deliver the necessary updates for the 1 July 2025 transition. These updates are designed to assist practices in identifying eligible patients, managing documentation, and maintaining recall processes.
MBS Item Changes
All new GPCCMP item numbers for GPs and Prescribed Medical Practitioners (face-to-face and telehealth video) will be available in Bp Premier from 1 July 2025.
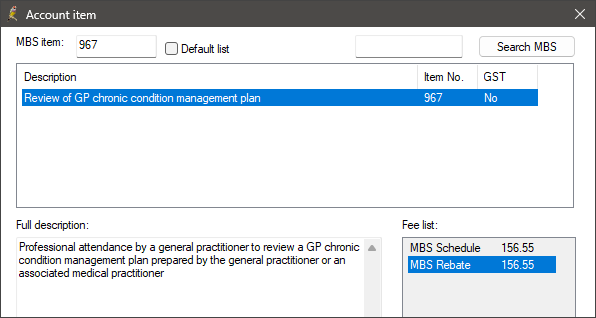
Visit the MBS Online website for more information on the MBS Items for GP Chronic Condition Management Plans.
Template Updates
Internal references in the existing system GPMP and TCA templates will be updated with GPCCMP terminology.
New Word Processor templates will also be provided for:
- GPCCMP Plan
- GPCCMP Allied Health Referral Letter.
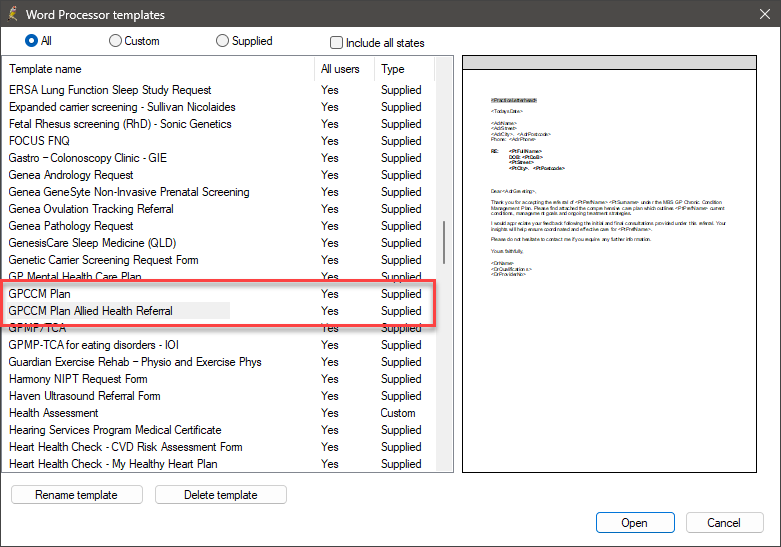
Custom templates will not be updated. Practices using their own templates should manually review and revise wording to match the new format and referral processes.
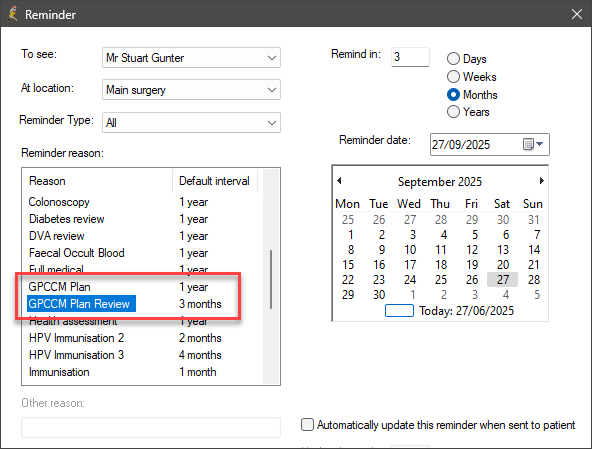
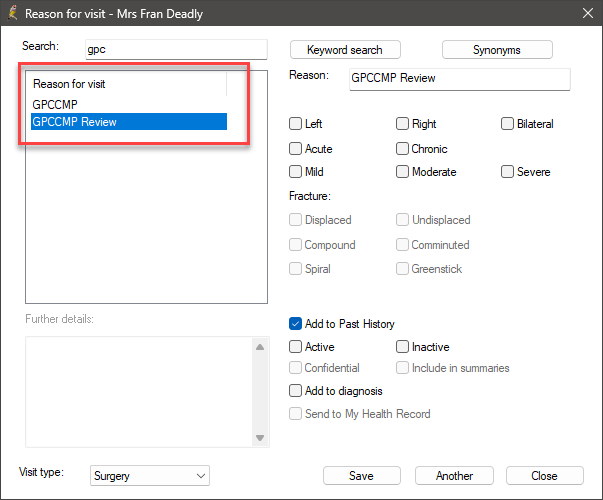
Reminder Reasons, Reasons for Visit and Appointment Types
New reminder reasons, reasons for visit and appointment types will be introduced to support patient recall and documentation for GPCCMP related appointments.
New Reminder Reasons
- GPCCMP Plan
- GPCCMP Plan Review.
New Reasons for Visit
- GPCCMP
- GPCCMP Review.
New Appointment Types
- GPCCMP Plan
- GPCCMP Plan Review.
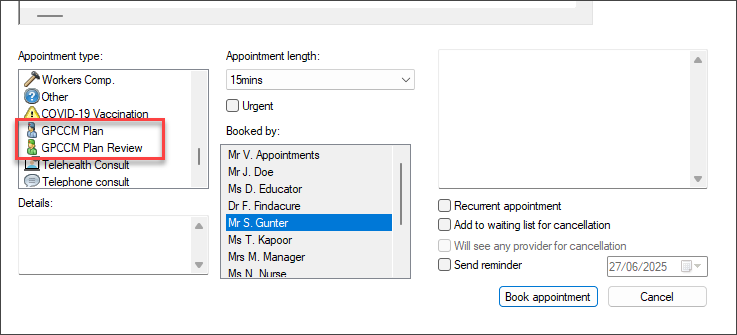
New appointments will default to twice the standard appointment duration; however, practices can adjust appointment lengths to reflect their clinical workflow preferences.
SQL Database Queries
To assist practices in identifying patients who may be eligible for MyMedicare or due for chronic condition management services, a series of SQL Search Queries has been made available for use in Bp Premier.
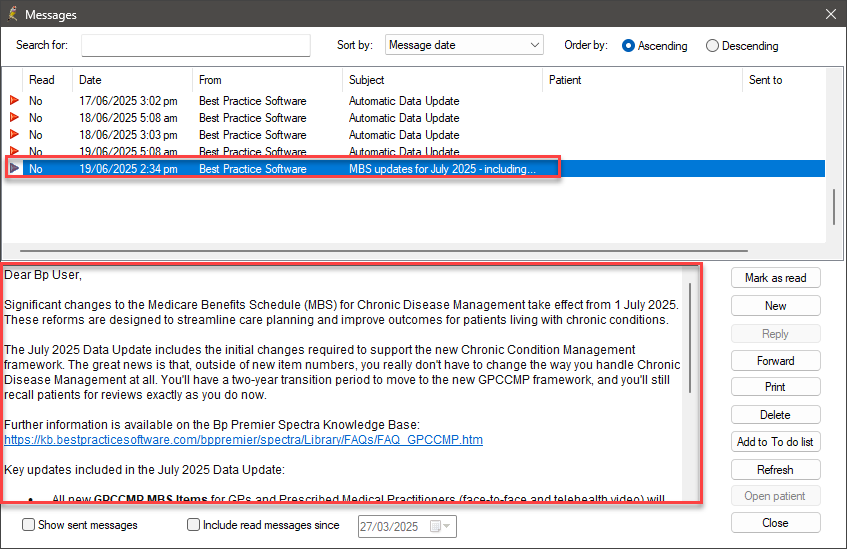
Internal Message Notification and Knowledge Base Links
Following the installation of the July 2025 data update, users will receive an Internal Message (F8) summarising the changes and providing direct links to Knowledge Base resources.
Enhancements in future versions of Bp Premier
Following the July 2025 Data Update, Bp Premier will continue to deliver enhancements through future program updates to support the full implementation of the GPCCMP model. These enhancements will introduce additional functionality to align with Medicare requirements and further streamline care planning, billing, and patient workflow management.
Co-claiming Logic
Bp Premier will introduce co-claiming validation to assist with billing accuracy when claiming the new GPCCMP items. The update will apply Medicare co-claiming rules for chronic condition items, including restrictions on billing preparation or review items alongside general attendance services on the same day.
This functionality is designed to reduce billing errors, support compliance, and streamline claim processing in Bp Premier.
EPC Module Updates
The EPC module will be updated to reflect the new GPCCMP terminology and planning structure. This includes revisions to care plan headers, referral documentation fields, and workflow prompts to align with the streamlined approach.
These changes will ensure practices can continue to document chronic disease management activity effectively using the existing EPC tools, with minimal disruption to established processes.
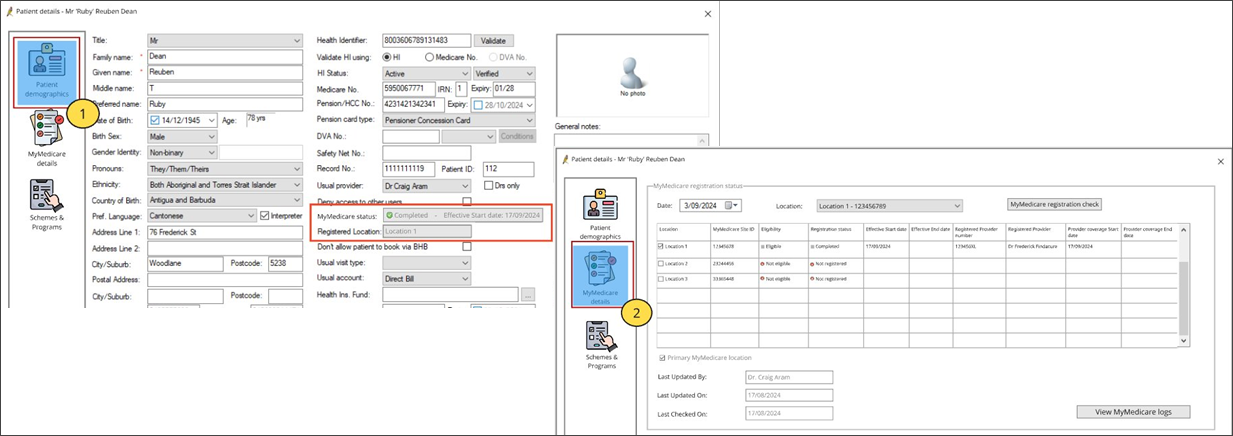
MyMedicare Medicare Web Services integration
A future version of Bp Premier will introduce functionality to manage MyMedicare registration information within the patient record. This will allow practices to:
- Confirm that GPCCMP services are billed through the patient’s registered practice in accordance with Medicare requirements.
- View and manage patient MyMedicare registration and enrolment.
- Confirm the patient’s eligibility for incentive payments.
The image below depicts an early design concept of the MyMedicare Medicare Web Services integration in Bp Premier. It is provided for illustrative purposes only and is subject to change as development progresses.
Next Steps
To ensure your practice is ready for the 1 July 2025 changes, Best Practice Software encourages practices to install the July 2025 Data Update as soon as it becomes available. You’ll be able to create the new GPCCMP for patients, bill the correct item numbers, and produce compliant referral documentation for Allied Health Services.
Information correct at time of publishing (27 June 2025).