This article offers answers to frequently asked questions as responded to by Dr. Fabrina Hossain, a Clinical Advisor at Best Practice Software, regarding Cervical Screening, with a particular focus on the Self-collection enhancements included in Bp Premier version Spectra SP1.
Cervical Screening results can be recorded into Bp Premier in the following areas:
- Main screen of Bp Premier > Clinical > Cervical screening
- Main screen of Bp Premier > View > Inbox
- Patient record > Cervical Screening
See Cervical Screening for more information.
Cervical Screening enhancements in Spectra SP1
What is the industry change behind the self-collection enhancements in Bp Premier version Spectra SP1?
Since July 2022, there has been the introduction of the 'self-collected' method of participating in the National Cervical Screening programme to test for the Human papillomavirus (HPV). Eligible women and people with a cervix between the ages of 25 – 74 can now opt to either have cervical cell samples collected by the doctor or nurse practitioner via speculum examination OR, IF they meet the suitability criteria, they can choose to have collected the less invasive 'self-collected' sample of vaginal cells which they can perform by themselves in private.
These changes were introduced to increase the participation of under-screened women, as the speculum examination can pose a significant barrier for some demographics. International studies have shown that providing HPV self-collection kits to never screened and under-screened women improved screening participation.
The Spectra SP1 enhancements will allow users to document in the Cervical Screening screen, if the Cervical Screening Test was a self-collected vaginal sample.

Why is it important to record if a cervical screening participant collected their own sample?
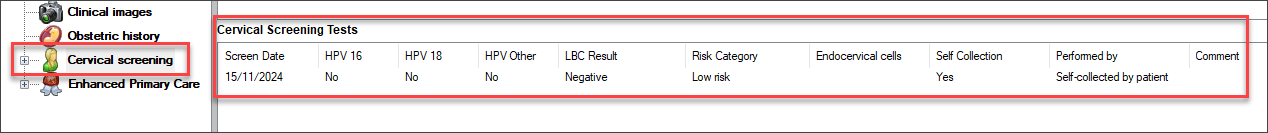
While most doctors would record in the patient's consult notes and pathology request form that the cervical screening test was a self-collected specimen, there are several advantages also to recording the results of the CST in Bp Premier's 'Cervical Screening' screen.
In my practice as a GP, I find the CST section to be a very quick and easy way to obtain many years of cervical screening results of the patient in one dedicated section of the software. This prevents the need to search through the investigations list to find CST results. The grid format provides a quick snapshot of the patient's cervical screening history that helps me to make clinical decisions efficiently.
Why is a clinician still involved in the process if it's self-collected?
A clinician is required to determine patient eligibility and suitability for a self-collected sample and to manage the outcome of the test result.
As pathology companies perform these tests, the request itself must be from a clinician to whom the results are sent for follow-up and further management. Also, it is important that patients who are at a higher risk of cervical cancer do not undertake a self-collected vaginal sample, as this test is designed for asymptomatic and low-risk individuals.
Is a self-collected sample as accurate as a clinician-collected sample?
Several international studies have demonstrated evidence to show Cervical Screening Tests using a self-collected sample, in appropriate population groups, are just as accurate at detecting HPV as a clinician-collected sample taken from the cervix during a speculum examination.
This is why it is important to ensure the patient satisfies the self-collection eligibility criteria.
For more information on patient eligibility for CST/HPV self-collections, visit the Department of Health and Aged Care website.
Why is it important to indicate that the clinician assisted with the self-collection?
Sometimes, patients are not physically able to collect their own sample, and request the doctor or nurse practitioner to assist them in the collection of the swab. In such cases, it is important to record the distinction between a vaginal sample collected by the patient themselves and a vaginal sample collected by the healthcare provider.
In the patient record, it's possible to indicate the clinician performed that collection, but also tick the self-collection checkbox. Can you describe the circumstance where Performed By Provider and Self-collected are both selected?
Some patients may wish to collect the specimen in the doctor's office behind a privacy screen or in the clinic restrooms. These swabs are then suspended in a collection vial at the time of collection. These tests are self-collected by the patient.
Sometimes, the patients are unable to collect the sample physically, so they request the healthcare provider to collect the sample for them. As the test is still a vaginal swab using a dry flocked swab, the sample type is still 'Self-collected', but the clinician performed it.
Finally, some patients may elect to conduct a self-collected sample in the privacy of their own home, in which case they will be given a different collection swab that they can drop off at the pathology centre. These tests are self-collected by the patient.
We have allowed for the distinction to be recorded in the CST section.
Enhancements to Database Search > Cervical Screening
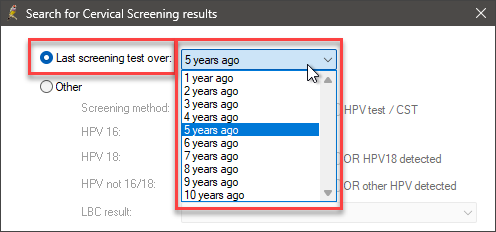
The time frame for searching for the last pap smear or cervical screening test has been updated from 2-4 years to include the last 1-10 years. What's the reason for extending the historical time frame?
Prior to 2017, Pap smears were conducted every 2 years for cervical cancer screening. Bp Premier was designed to search by these increments. However, with CST screening now performed every 5 years, we have extended the time frame to allow for more accurate searching of under-screened patients.
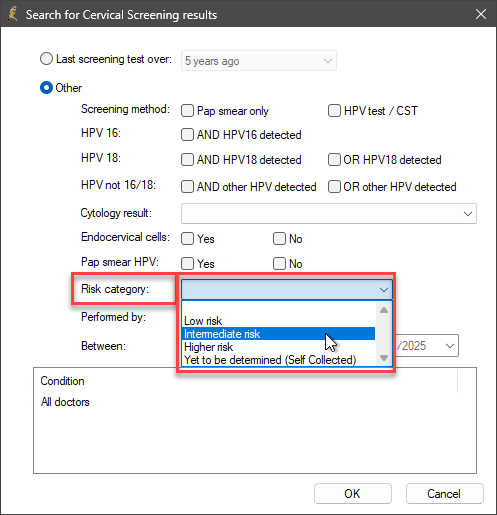
The risk category has been added as a search option. Could you explain why you would select 'Intermediate' when searching for self-collected cervical screening tests?
Users can now search for risk categories. If you wanted to conduct a follow-up audit on all of the patients with 'Intermediate' risk to ensure they had had their 12-month follow-up test, you would select 'Risk category > Intermediate'.
Information correct at time of publishing (29 January 2025).