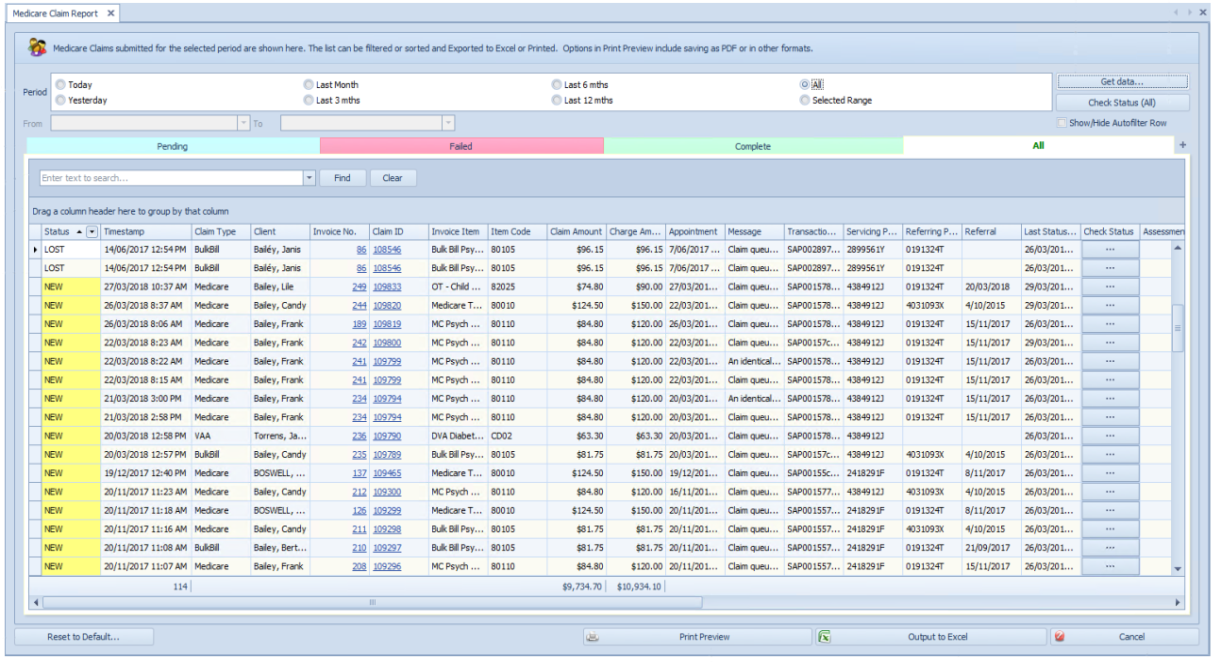
The Medicare Claim History report displays any claims that have been submitted to Medicare via Patient, DVA or Bulk Bill claiming.
- Locate Reports from the left-hand menu in Bp Allied.
- Select Medicare.
- Select Medicare Claim History Report.
|
Field |
Description |
|---|---|
|
Select a date range |
Enter the date range to find claims for. Clicking on Selected Range enables the From and To date fields. |
|
Get Data |
Click Get Data to search for claims for the date range above. |
|
Process Flow |
Pending – shows claims that have been sent to Medicare but not yet paid. The most recent claims are displayed at the top. Failed – shows any claims that have been Delayed, Rejected or Lost. Claims are able to be resubmitted from this screen. Complete – shows all completed claims. All – shows all claims. + - can be clicked to include any claims that failed to be sent to Medicare because they were rejected at the time of submission. These display within the ALL tab only. |
|
Find a claim |
Use the Find field to search for a particular word within the report, i.e. to find a particular item. |
|
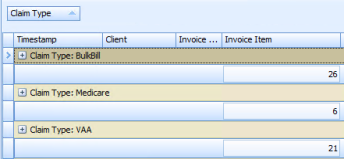
Group by.... |
Use the Group By option to group the claims entered. An example would be to drag the Claim Type field upto the Group By header so that the claims can be displayed by type.
|
|
Reset to default |
Resets the columns under each tab to the default layout. |
Check Status
Checks the status of all claims. Use this to find out if a claim has been paid or not.
|
Field |
Description |
|---|---|
|
New |
The initial status for all claims. |
|
With Medicare |
Status for DVA, Bulk Bill, once submitted. Note, if a claim stays at With Medicare for more than a week, it can be worth calling Medicare to find out why there is an issue with the claim. Because the claim is with Medicare and has stalled there is no information that we can pass back in an automated manner. |
|
Invalid |
There is a problem with the claim at time of submission. There is usually a message that pops up for the user at submission time so that they can review and fix the data and resubmit the claim. See the message field for details of what the issue is. |
|
Processed |
If an organisation is paying a benefit, it sits at processed until it is paid. |
|
Complete |
When a claim has been paid. If the benefit various organisations will pay for the claim = $0, the claim will be marked as COMPLETE and no more information is expected. If a DVA kilometres claim has been paid, the relevant Invoice will be updated. |
|
Delayed |
There is some other error with the claim, for example: error 9201 – Invalid format for data item. This is an error indicating that the pre-processing has found an error in the format of some element(s) in the claim. E.g with the format of the client's name. |
|
Rejected |
This means claim was rejected by Medicare (“benefitPaid”: 0) with assessment error code based on the standard Medicare rejection codes (link below). |
|
Lost |
When we successfully submitted the claim to Medicare but there was no response after 14 days, we change the status to LOST. There’s nothing at Medicare for us to retrieve and report on. Almost always this means the provider paperwork is not submitted or not yet processed. |
Medicare and DVA troubleshooting resources can be found in the following links:
- Medicare reason codes and reducing claim rejections
- Medicare digital claiming return codes
- DVA reason codes
Fields available to be reported on include:
|
|