On this page:
Failed, lost, delayed bulk bill and delayed DVA claims can be resubmitted. Patients must contact Medicare regarding any Patient Claims with a permanent status of “With Medicare”. These claims can be resubmitted using the manual decline function in the Medicare Claim History Report. See Manually Decline a Claim for more information.
Resubmit a claim
- Locate Reports from the left-hand menu in Bp Allied.
- Select Medicare.
- Select Medicare Claim History Report.
- Select the relevant time period and click Get Data.
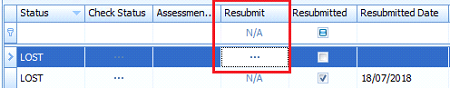
- Select the Failed tab.
- Find an item to be resubmitted and select the ellipsis [...] button in the Resubmit column.
- This action will either:
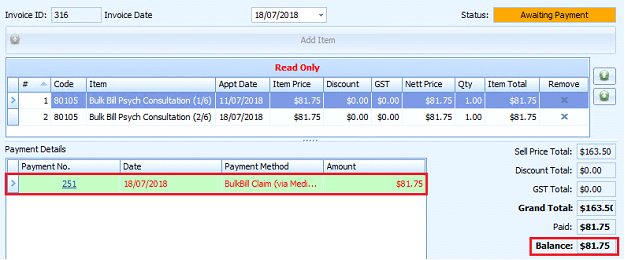
- Open the relevant invoice in Invoices
- Zero the current payment against the invoice
- If more than one item is on the Invoice, the payment balance is adjusted to the amount paid.
- The text in the payment line will turn red.
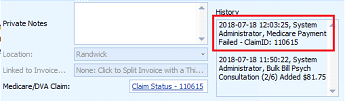
- A note will be added to the Invoice History to record the change.
- From the invoice, click Add Payment.
- Only the balance due to be paid will display in the Payment Amount.
- Click OK.
- Continue to process the payment or claim as usual.
If a payment type of Bulk Billed or DVA claim is selected:
- Only the unpaid Bulk Bill or DVA Item will be resubmitted. In the Medicare Claim History Report, the Resubmitted check box is ticked and the Resubmitted Date added for the original claim.
- The Claim History Report shows a link in the Link to Record field to the original claim.
- The Claim Number is updated on the Invoice to the new Claim Number.
If another type of payment is selected, this will be processed as usual:
- No changes are made in the Medicare Claim History Report.
- It is advised to enter a note against the original claim to record how the payment has been received.
TIP If payments are regularly received via a manual Bulk Bill or DVA process, a Payment type of Manual BB or DVA claim can be added to track these if necessary. See Payment Types for more information.
Original invoice or claim is no longer valid
When the original claim or invoice is no longer valid a workaround must be carried out.
- Resubmit the claim as outlined above without adding payment.
- Update the Item Price in the Invoice Line item to $0.00.
- Click Save.
- Record this process in the Invoice Private Notes and Medicare Claim History Report notes for future reference.
Resubmit a Bulk Bill claim with an item price different to the current price
When resubmitting an older claim, the price of an item claimed can change between when it is submitted and when it is rejected by Medicare. In these cases, the claim must be resubmitted at the original price.
The process is the same as a normal resubmission, with some notable differences:
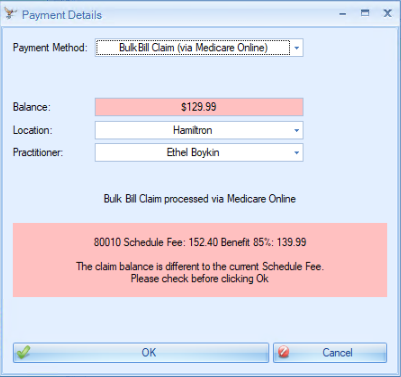
- Clicking on Resubmit in the Claim History report will set the previous Bulk Bill payment to $0.00.
- The Invoice status will change to Draft.
- After resolving the invoice or claim error, re-add a Bulk Bill Payment. A warning will display 'The claim balance is different to the current Schedule Fee'.
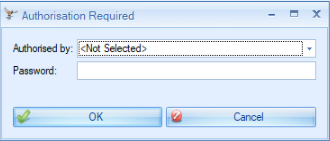
- Click OK. The Authorisation Required window will display.
- Enter the authorisation details and click OK to process the Bulk Billed claim. The claim resubmission process will continue as normal.
NOTE Claims can be resubmitted multiple times.
Update the item claimed on an invoice as part of a resubmission
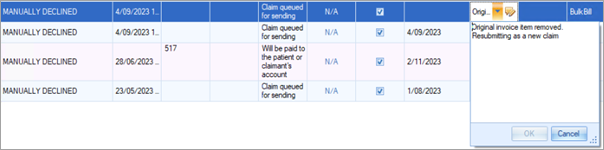
Some claims are rejected due to an incorrect item number claimed on the invoice. In previous versions of Bp Allied, removing the incorrect item from the invoice would delete the related claim from the Claim History Report. The record would still appear in the Audit Log.
In Bp Allied V7 SP3 Revision 1, removing an incorrect item from an invoice will unlink the claim in the Claim History Report from the invoice but not deleting it. The records will be retained in the Claim History Report for auditing purposes.
- Clicking on Resubmit in the Claim History report will set the previous Bulk Bill payment to $0.00.
- The Invoice status will change to Draft.
-
The incorrect line item can be removed from the invoice and a new item can be added.
- If the new item price is different to the current price, The 'Claim balance is different to the current Schedule Fee'. message will display, and authorisation is required to process the Bulk Bill claim.
- If the new item price matches the MBS schedule fee, no message is displayed.
- The claim with old item will remain in the Claim History screen, with a note added 'Original invoice item removed. Resubmitting as a new claim'. There will be no resubmission date, as that claim is not resubmitted. The original Claim ID will be listed in the Invoice History notes.
NOTE Claims can be resubmitted multiple times.
Last Updated 12 December 2023