The Tyro HealthPoint Claims report displays all claims lodged by Bp Allied during the period of time selected. It does not include any quotes requested. This information can be view against the quote or from the Quote Summary report.
If a claim has been lodged multiple times, for example lodged and Accepted by the Client, and then Cancelled in the same day, two lines will display in the report. One with the Claim Status = Approved and a second one with Claim Status = Cancelled. Both will be linked to the same Invoice ID.
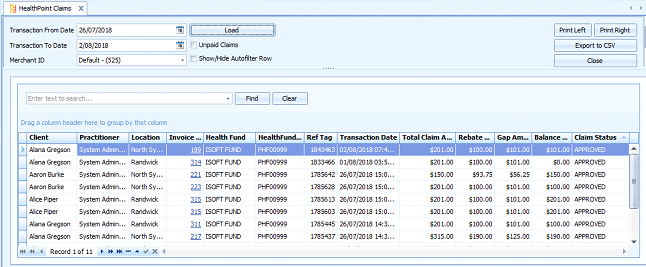
To run the report
- Select Reports > Tyro > HealthPoint Claims.
- Select the relevant Transaction From Date and Transaction To Date.
- Select the relevant Merchant ID (MID).
- Click Load. All the claims for the selected time and MID will display.
- Click Unpaid Claims checkbox to view only claims with an outstanding Balance Amount.
- Use the standard grouping and filtering functions to group claims by HealthFund, Practitioner, Claim Status or Location as required.
Additional Merchant IDs will only be seen where there are Practitioners with their own MID within the practice and these are accessed via the same terminal as the MID registered to the practice.
Definition of fields displayed:
- Client – the client that the claim has been lodged on behalf of
- Practitioner – the practitioner who provided the service to the client
- Location – the location of the service
- Invoice ID – the Bp Allied Invoice number that holds the details of the claim. View the invoice by clicking on the link.
- Health Fund – the Health fund that the claim has been lodged with. This is determined by the fund associated with the Client.
- Health Fund ID – the unique number assigned to the Health fund
- Ref Tag – the unique number assigned to the claim by HealthPoint. Use this number if raising an issue about a claim payment with Tyro.
- Transaction Date – the date the claim was lodged
- Total Claim Amount – the total amount the practice charges for the services lodged
- Rebate Amount – the total amount that the Health Fund will pay on all the services on the claim lodged including any loyalty payment. View the individual claim information on the related invoice to details of the individual amounts.
- Gap Amount – the amount of the claim that needs to be paid by the client
- Balance Amount – the amount left to be paid
- Claim Status – the overall status of the claim as lodged with Health Point.
- Claim Statuses are:
- APPROVED – Claim was Approved by the Health Fund and Accepted by patient
- VOIDED – Claim was Approved by Fund and Rejected by patient
- CANCELLED – Claim is already cancelled
- RECONCILED – Claim is already settled (Claimed prior to this day)
- DECLINED – Claim was declined by the Health Fund
- FAILED – an error occur during processing of the Claim, system Void