This article explains how to modify a claim that has been returned from Medicare with a "MEDICARE_PENDABLE' status, indicating that the original invoice must be updated with supplementary information for operator assessment. Pendable claims should be actioned and resubmitted as they return after submission.
See Pendable to pended invoices and Medicare Web Services for more information.
- Select the Invoice with 'EZ' displayed in the Batch column and click Modify.
- If you are selecting conditions for the invoice, such as Not Duplicate Service or Multiple Procedure override, click the chevron button < at the end of the item row in F5 to open the Medicare Consultation Item details screen.
- Add all required additional information and service text and click OK to return to the Consultation screen.
- Medicare Authorised cannot be unselected as this claim is already in Pendable status.
- Click the red Medicare button on the Consultation screen. The Patient Claims screen is displayed.
- Click Send Claim. The claim will send to Medicare with a MEDICARE_PENDED status as the claim is still requiring manual assessment by Medicare.
Most details can be modified from the Consultation Screen including the Service Date, Provider, Items and additional Medicare Consultation Items.
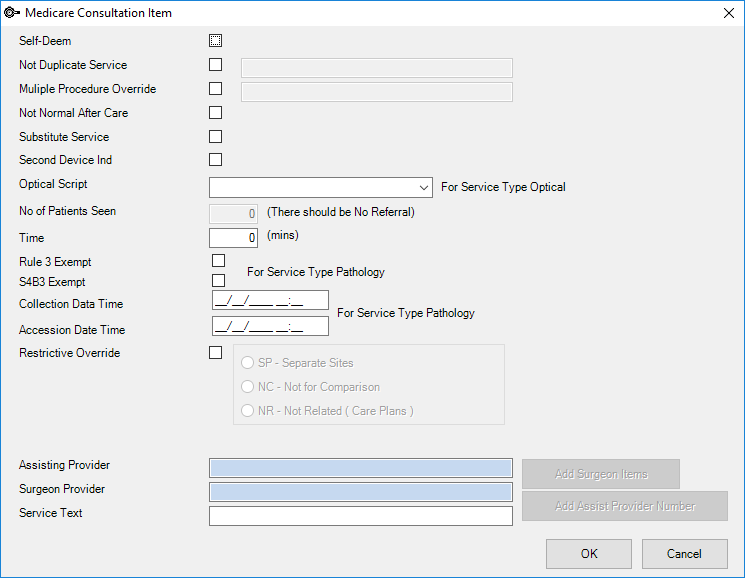
Notes added into related text fields will be sent to Medicare, providing evidence for the selected condition. The Service Text field at the bottom of the screen will also transmit to Medicare.
You cannot modify the invoice from this point, as the invoice has now been transmitted to Medicare. As the invoice has had the status of Pendable, been modified, and then sent as a Pended claim, the claim is not displayed in the Same Day Delete screen.
You will need to contact Medicare directly if there are any issues with a MEDICARE_PENDED status claim.
Last modified: 05 May 2022