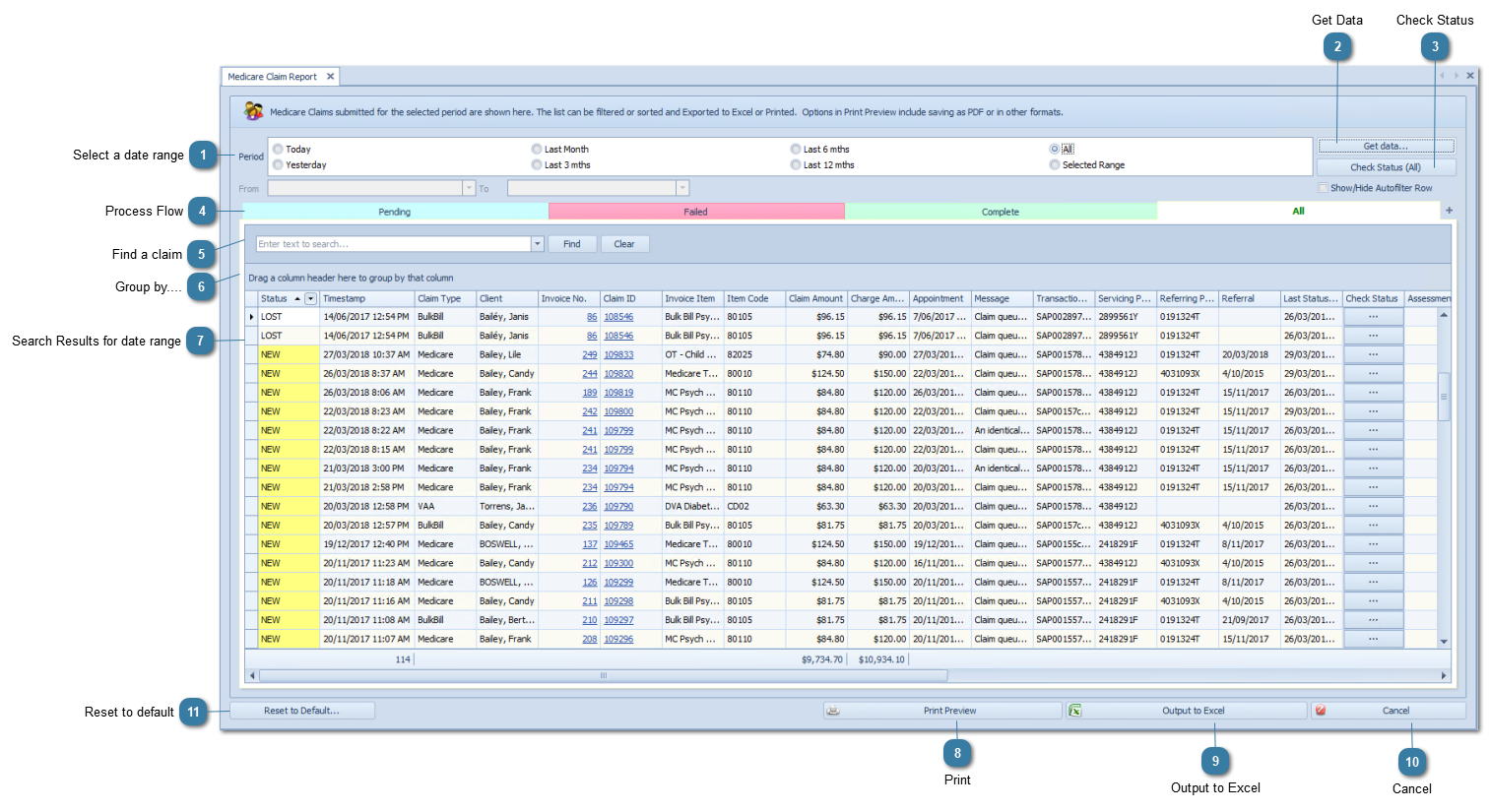
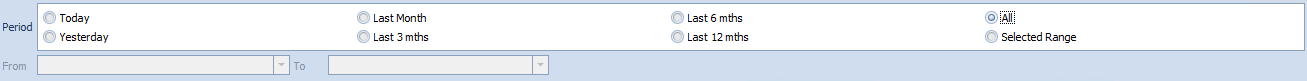
Search Results for date rangeSearch results for the above date range.
Fields available:
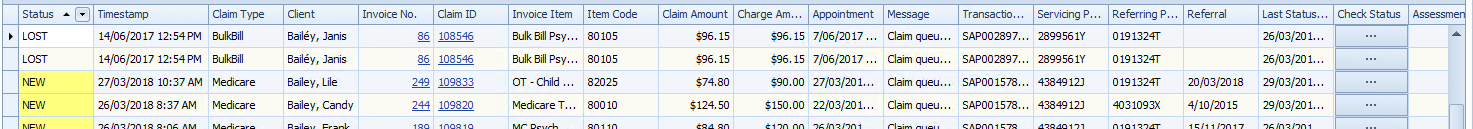
Timestamp - date and time the claim was sent
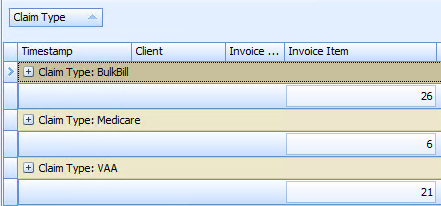
Claim Type - whether its Bulk Bill, VAA (DVA), Medicare (Patient Claim)
Client - who the claim is for
Invoice No. - Invoice claimed
Invoice Item - Item description
Item Code - Medicare or DVA Item Code
Claim Amount - Amount claimed
Charge Amount - Amount charged. For DVA and BB this must be the same as Claim Amount
Appointment - Appointment Date and Time
Claim ID - Claim ID assigned by Bp Allied
Message - any error messages relating to the claim will be stored here. If it has been successfully sent then the message is "Claim queued for sending"
Transaction ID - ID assigned by Claiming.com.au
Servicing Provider ID - The provider number of the medical practitioner rendering the service(s) as allocated by Medicare
Referring Provider ID - The referring provider number
Referral Date - The date the referral was issued
Last Status Check - date and time when the status was last checked
Check Status - Click to check the status if an individual claim
Assessment Note - Includes any rejection codes that come back from Medicare if the claim could not be successfully processed
Benefit Paid - amount paid by Medicare or DVA. This could include Loading and KM payments
Status – as above, the current status of the claim
Benefit Assessor – whether the claim has been assessed by Medicare or DVA
Assessment Note Code – Code returned from Medicare or DVA if the claim has been failed
Assessment Note Assessor – ID of the person that has assessed the claim at Medicare
Payment Run – payment batch number from Medicare
Practitioner – Practitioner assigned to the invoice that was claimed.
Notes – notes can be added if claim needs to be resubmitted
Resubmitted – checkbox is ticked if the claim has been resubmitted
Resubmitted date – the date resubmitted (if relevant)
Payment No – link to the payment record
Link to Record – links to original claim if this claim was one that was resubmitted
|