These release notes describe all enhancements and modifications made to Bp VIP.net since version Topaz (2.1.526.051).
|
Release Date |
31 May 2022 |
|
Release version |
Topaz Service Pack 1 (version 2.1.529.008) |
|
Notes last updated |
31 July 2022 |
|
What is in this release? |
Bp VIP.net2.1.529.008 contains: Medicare Web services integration for Australian practices; Xero integration updates; and other enhancements and bug fixes. |
|
Which version can I upgrade from? |
There is no version dependency for upgrading to 2.1.529.008. Topaz SP1 requires Microsoft .NET Framework 4.8, If you are running a .NET version earlier than 4.8, you must upgrade .NET on the server and all workstations before you can start using Topaz SP1. |
|
When should I upgrade? |
Best Practice Software recommend running the program upgrade outside of business hours to minimise the impact of the upgrade on your practice. |
|
How do I upgrade? |
Upgrade instructions are included in these release notes:
|
|
What do I do after upgrading? |
Before you can claim through Medicare Web Services after upgrading, register your B2B devices in PRODA, and switch on this function in Bp VIP.net. |
Upgrade Bp VIP.net to Topaz Service Pack 1 (2.1.529.008)
You should be able to upgrade to 2.1.529.008 from any version of Bp VIP.net. Best Practice Software recommend that the upgrade be performed outside of normal business hours.
Notes on upgrading
- If you did not upgrade to the most recent version, Topaz 2.1.526.051, review the release notes to see the changes in that version.
- Copy the install file to and run the upgrade from the PC running the SQL Server database first. This will upgrade the Bp VIP.net database structure in preparation for terminal server or workstation upgrades.
- If your practice uses Terminal Services, you must run the installation from the Terminal Server (after upgrading the database server).
- Log in to the Bp VIP.net server computer as a Windows administrator. You may require Windows administrator permissions to install and update some Bp VIP.net components.
- After you upgrade to Topaz SP1 and switch on Medicare Web Services, you will be unable to resubmit amended claims or batches that were sent before you enabled MWS. Best Practice Software recommend that you reconcile all batches and claims sent before carrying out step 4 below.
1. Set up PRODA Account
Best Practice Software recommend that your practice set up a PRODA account before you upgrade to version Topaz SP1. Learn more about PRODA from the Service Australia website.
2. Upgrade to version 2.1.529.008
- Check the version of Microsoft .NET Framework on the Bp VIP.net server and workstations. Topaz SP1 requires a minimum .NET Framework version of 4.8.
- Back up your existing database before upgrading and test that the backup restores successfully. Information on how to back up and restore your database is available on the knowledge base.
- Download the setup.zip file here. Your browser may warn that the file is a security risk. You can safely keep this file.
- Copy the setup.zip file to the folder nominated in Setup > Facility Preferences > General Preferences > Login/Tasks tab > New version location field. This field must contain a UNC path to a network location accessible by Bp VIP.net workstations.
- Log in to the database server as an administrator user. Bp VIP.net will detect that a new setup.zip file exists and begin upgrading the server and database.
- When a user next logs in to a workstation, Bp VIP.net will detect that a new setup.zip file exists in this folder and will automatically upgrade the version of Bp VIP.net on the workstation.
- If your practice uses a MIMS database, check your version of MIMS and update to the latest version if available.
3. Register B2B devices
You must register all PRODA organisations that will submit claims from your practice as a 'B2B Device' in Medicare Web Services. You do NOT need to register a B2B device for each Minor ID or Location at your practice. B2B device registration is influenced by organisation structure, not practice location.
For more information on how to register B2B devices, select Help > Online in Bp VIP.net to open the online Knowledge Base and search for 'mws'.
4. Enable Medicare Web Services
IMPORTANT Before enabling MWS in Bp VIP.net, reconcile all outstanding batches and claims.
If you must reconcile a pre-upgrade batch after you upgrade, you may have to temporarily disable MWS while performing the reconciliation and resubmission.
If you are satisfied that your practice has completed all the prerequisites, you can now enable MWS.
- Log in to Bp VIP.net as an administrator with access to Setup.
- Go to Setup > Facility Preferences > General Preferences > Facility tab.
- Select 'Yes' under Use Medicare Web Services and click OK.

Bp VIP.net will begin using the MWS framework for claiming. Ensure that your billing staff are familiar with the new MWS billing workflows and messages.
IMPORTANT Best Practice Software strongly recommend that you complete all prerequisites and enable MWS before the cutoff date of 19 June 2022. If you have not enabled MWS in your database by this date, you may require assistance from Bp VIP.net Support to enable this feature. Medicare and DVA claiming through the old 'adapter' technology will not be possible after this date.
Medicare Web Services changes
Services Australia is upgrading the technology used by Practice management software for digital health services, such as online verification and claiming, from an adapter-based technology to 'Medicare Web Services', a secure framework for online communications over the Internet.
Version Topaz Service Pack 1 (SP1) supports the new Medicare Web Services technology for all Medicare and DVA online verification and claiming. Bp VIP.net practices must update to Topaz SP1 before 19 June 2022 to continue to use these functions after this date.
Medicare Web Services has required some changes to claiming workflows, patient statements (such as Lodgement Advice) , and alert messages received from Medicare and DVA during claiming. Your billing staff should familiarise themselves with the workflow changes in this release. Changes that affect workflows have been summarised in this section.
Review the New Features table for more information on Medicare Web Services changes to Bp VIP.net.
Practices with multiple locations or B2B devices
If your practice has multiple locations or 'facilities' where each location has a distinct Minor ID, or your organisational structure requires more than one B2B device registered, when you initiate any Medicare Web Services transactions from Bp VIP.net, such as verification or claiming, the Bp VIP.net user will be presented with a new PRODA Login popup:
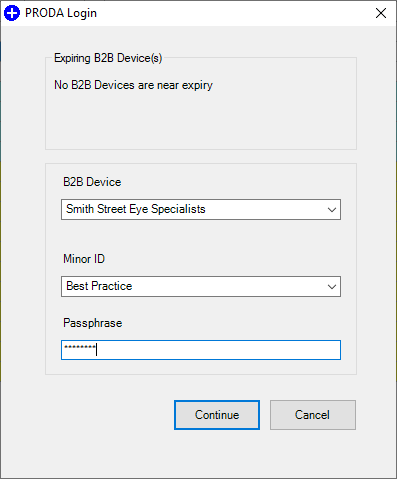
Select the B2B Device (organisation) and Minor ID (Location) to conduct the transaction for.
Payment and Processing Report Return Messages
When you request a payment or processing report for bulk bill or private claims, the messages returned under Medicare Web Services have changed and may be unfamiliar to your Bp VIP.net operators. The following table contains more information about report request statuses:
|
Message |
Description |
|---|---|
|
REPORT_NOT_FOUND |
Generated by the following scenarios:
For multi-location practices, ensure that the user requesting the report selects the correct B2B device when entering the Medicare Service options screen. Otherwise, you must contact Services Australia for more information to resolve the issue. |
|
REPORT_EXPIRED |
The report request is more than six months from the Date of Lodgement of one or more claims. Check the request reporting period. |
|
REPORT_NOT_READY |
The claim has not yet been finalised by Services Australia. Try again later. |
|
REPORT_NOT_AVAILABLE |
The claim was processed and has been rejected. Check the processing report for more information. |
|
READY |
The report is available for retrieval. |
|
REPORTED |
The claim has already been reported. |
Pending statuses
Two new Medicare claim statuses for Patient Claiming Interactive (private) claims may appear for submitted claims after you upgrade to Medicare Web Services in version Topaz SP1: 'pendable' and 'pended'.
If a claim requires supporting information, such as service text or a Not Normal Aftercare indicator, the claim may require an operator to check the supplementary information provided with the invoice before the claim can be accepted. If this is the case, the invoice will return with the status of PENDABLE (or MEDICARE_PENDABLE) indicating the invoice details should be reviewed for completeness before resubmission.
Resubmitting a pendable claim will update the status to PENDED.
Best Practice Software recommend actioning PENDABLE claims and resubmitting the invoice immediately if an invoice is returned with PENDABLE, rather than reviewing such claims as an end of day activity.
The Patient Claims report (Financial Reports > Patient Claims) has been updated with options to report on claims with a status of pendable or rejected to assist in locating and actioning these claims.
For more information on the pendable to pended workflow, select Help > Online Help from within Bp VIP.net to open the Bp VIP.net Knowledge Base and search for 'mws'.
Batch number changes
As part of Medicare Web Services changes to claiming workflows, bulk bill claim numbers reset to start at 'A0001' every day, for each provider. This change may require your practice to update its method for locating services in a batch for reconciliation.
The Search function from the Transactions history screen (F8) now allows you to search by:
- Batch Number. This can be further refined by providing a Provider name and batch Date.
- Correlation ID. The Correlation ID is a unique identifier for a Medicare Web Services transaction. This value may be supplied by Services Australia in a processing report or reconciliation correspondence.
For more information
For more information about Medicare Web Services configuration and usage in Bp VIP.net, select Help > Online from within Bp VIP.net to open the Knowledge Base, and search for 'mws'.
Information is also available from Service Australia's website.
Inpatient Eclipse claiming
Private inpatient claims can now be transmitted as an IMC (Inpatient Medical Claim) for patients who are not eligible under their health fund to claim for the specified service. The patient pays the full amount and is rebated the Medicare subsidy by Medicare.
Previously these could only be transmitted using the PCI claiming functionality.
For more information on these claims, select Help > Online Help from within Bp VIP.net to open the Bp VIP.net Knowledge Base and search for 'IMC PC'.
Manual batching
You can now manually create batches of items from the Batch Preview screen. In prior versions, users had to contact Bp VIP.net Support for assistance creating a manual batch for items still inside the two-year window for submission.
In Topaz SP1, the Create Manual Batch button is available from this screen to select items for a manual batch:
- Items added to manual batches are excluded from any other transmissions to Services Australia
- A batch number is generated by Bp VIP.net and can be used as a batch reference for processing and payment reports
- Manual batches in the Transactions screen (F8) have an 'M' in the Batch column.
If you accidentally create a manual batch, you can delete the batch and release the items back to the Batch Review screen.
Xero integration
Bp VIP.net can export financial data to the accounting software Xero. Revenue transactions are conducted in Bp VIP.net, but the data export transfers transaction data to your Xero account for more complex billing and analysis.
Version Topaz Service Pack 1 restores the ability to create a scheduled task to export financial data to a Xero account. Scheduled exports to Xero were temporarily unavailable in version Topaz.
Failed Xero scheduled export tasks are left with a status of 'incomplete' and are marked 'urgent' for user attention in version Topaz SP1.
For more information on the changes to Xero integration in this version, select Help > Online from within Bp VIP.net to open the Knowledge Base, and search for 'xero'.
New Features
|
Function |
Release Notes |
Key |
|---|---|---|
|
SMS |
When sending bulk SMS, the option Hide Inactive is now available to remove inactive locations from the list to send SMS messages from. |
55011 |
|
Reporting |
In the Referrers Report, the Clinic name is now displayed in front of the Provider's address section on screen and in report exports. |
26705 |
|
Reporting |
A new column Mobile has been added to the Appointment Book Summary Report which shows the patient's mobile phone number. |
68923 |
|
Reporting |
A new column Mobile has been added to the Next Appointment Recall Report which shows the patient's mobile phone number. |
68924 |
|
Reporting |
The Patient Claims report (Financial Reports > Patient Claims) has been updated with options to report on claims with a status of pendable or rejected to assist in locating and actioning these claims. |
69004 |
|
MyComms |
A new Ctrl-L lookup field has been added: Name & Address / Known Name (Bracketed). This field will print Title Firstname (Known name) Surname. |
68073 |
|
Setup Charges |
A new option Item Ordering has been introduced to Fee Setup for Subsidisers. Users can now choose whether to follow standard Medicare rules for ordering items in Consultation (F5), or order items by highest to lowest subsidiser fee only. |
64354 |
|
Patient Claims |
For PCI and IMC-PC claims, the age at which a claimant or redirector is required has been raised from 12 to 14. The age up has been updated in relevant user notifications. |
68603 |
|
Aged Debtors Report |
When running aged debtors for a subsidiser with batches, the report grouped any duplicate batch numbers from Medicare. Now, if 'Debtors' is selected for the Groups filter, batches are displayed independently. Date and Owed Provider details have been added to the report for clarity. |
68537 |
|
Bulk Bill batching |
In the Batch preview screen, the button Create Batches is now labelled Create/Send Batches. This function now both batches and sends a batch at the same time. From the Medicare Service options screen, option 4. Create and Send Batches now also performs both functions. You no longer have to send batches from 5. Bulk Billing Claims or 6. DVA Paperless Streamlining Claims. |
67881 |
|
General errors |
Errors of return code 500 indicate a problem with the Internet connection with Services Australia and now return an error message indicating that users should contact Medicare for support. |
66660 |
|
Help menu |
The toolbar Help Menu has been updated to reflect recent changes. Obsolete options have been removed and the Help link to the online knowledge base has been renamed to 'Online Knowledge Base'. |
68049 |
|
In-Hospital Claims |
Critical Care Service has been added to the Consultation Item popup from the Consultation screen. The checkbox allows the user to select which item is included as the critical care item. |
68813 |
|
In-Hospital Claims |
The list of options for Same Day Status Code has been updated for IHCW Claims . |
68749 |
|
In-Hospital Claims |
Changes have been made to the Medicare In Hospital Claims screen. Almost all of the fields on this screen are populated from operation details and the Day Stay Episode, alterations from this screen are not preserved. These fields are now read-only to reflect this. |
67711 |
|
In-Patient Medical Claims |
A new checkbox Include Billing Agent No has been added to the IMC Claims screen. The checkbox is ticked or unticked by default based on the selected Claim Type, and cannot be modified for claim types of 'PC' or 'MB'. If ticked, the billing agent provider number is sent with the claim. |
68351 |
|
In-Patient Medical Claims |
For IMC Claims of type 'SC' (Scheme), Bp VIP.net now alerts the user if the Financial Interest Disclosure and Informed Financial Consent options are not correct for the SC claim type. |
68435 |
|
In-Patient Medical Claims |
The label for Informed Financial Consent options is now clearer. |
-- |
|
Logging |
PRODA and Medicare Web Service transaction logs are truncated to the most recent 8 weeks. |
67458 |
|
Medicare and DVA documents |
Service detail codes and related values if present (such as indication of aftercare, or multiple services) are printed at the end of the relevant service description in the Lodgement Advice or Benefit of Statement and Claim. |
67538 |
|
Medicare and DVA documents |
For Bulk Billing, if time duration, accession date or collection date is set, these details are printed on the statement for the relevant service at the end of the service description. |
67596 |
|
Medicare and DVA documents |
The Patient Claim Consent and Declaration form for In-patient Medical Claims has been updated in accordance with changes for Medicare Web Services. |
64707 |
|
Medicare, DVA , and Health Fund Reports |
The format of the Online Eligibility Check (OEC) report has been updated for Medicare Web Services. This report contains new details on Health Fund and Medicare status information if available. |
67924 |
|
Medicare, DVA , and Health Fund Reports |
In DVA and DVA Allied processing reports, for items where the charge amount is equal to the claim benefit (that is, the item was fully paid), service details for the item will no longer appear. Processing reports will only show unpaid or partially paid items. |
-- |
|
Medicare, DVA , and Health Fund Reports |
When running IMC, IHC, or OEC reports (Processing, Payment, Declines), Location and Provider filtering (top right options) in these screens has changed. The Minor ID/Location field displays the location of the logged-in user (single Location) or the B2B and Minor ID (multi-location practice) selected and cannot be changed. You can select an Individual Provider if you wish to filter reports to a single provider. |
67398 |
|
Medicare, DVA , and Health Fund Reports |
When generating IHC or IMC payment and processing reports, you can filter the reports to a single Health Fund from the Fund field. |
67396 |
|
Medicare, DVA , and Health Fund Reports |
The IHC Processing Report has been updated for Medicare Web Services. Some field labels have changed, and Fund Status has been added. |
65142 |
|
Medicare and DVA |
In the general Medicare Service options screens, option 4 Process Stored Claims has been renamed to Create and Send Batches and now links to the same screen as File > Communications > Subsidiser Batching. You can no longer store claims for later submission in accordance with Medicare Web Services updated functionality. |
68065 |
|
Online Verification |
When a verification check is run for either Medicare only or Health Fund Only, the last verified date is updated and refreshed. |
65265 |
|
Patient Claiming |
IMC-PC is for claiming the rebate from Medicare, where the patient is not eligible under their healthfund to claim for a particular service. Pre-requisite for this type of claim is that the patient must have a health fund and details recorded on the F3 screen. IMC Patient Claims are submitted from Bp VIP.net, for invoices owed to the patient or redirected patient, not Medicare/DVA or Health Fund. A new checkbox IMC PC is available on the Consultation (F5) screen to indicate this claim type if:
The Account Paid checkbox on the Medicare Service screen is ticked and read-only for fully paid IMC PC claims. |
68072 |
|
Patient Claiming |
The user is now alerted when attempting to send an SC (Scheme/Contract) type IMC claim and hasn’t selected a Financial Interest Disclosure (FID) option. |
67317 |
|
Patient Claiming |
The user is now alerted when attempting to send a claim of type AG (Agreement) and hasn’t selected an Informed Financial Consent (IFC) option. |
67318 |
|
Patient Details |
Online verification buttons in this screen have been relabelled to better reflect the Services Australia function being used. |
-- |
|
Patient Statements of Claim and Benefit |
If time duration, accession date or collection date is transmitted for relevant Bulk Bill claims, these times are included in the service description and printed on the patient statement. |
67596 |
|
Payment (F6) and Transactions (F8) |
The fields VIP EasyClaim Authorised and EasyClaim Authorised in these screens are now labelled 'Medicare Authorised'. |
-- |
|
Search (F2) |
You can now search for patients by patient email address, recorded in Patient Details (F3). Prefix the search term with '@'. |
27539 |
|
Service Details |
The HIC Consultation Item window for entering service details from the Consultation screen has been renamed to Consultation Item and the fields rearranged for clarity. |
-- |
|
Xero integration |
Scheduled task functionality has been restored to practices that have a Xero integration with Bp VIP.net. Some limits apply:
If you haven't run a successful export for seven days, you will have to run a manual export to restart the check timer. Best Practice Software recommend that tasks are regularly reviewed to check for incomplete exports. |
65520 |
|
Transaction History (F8) |
The Status field in the footer of the Transactions history screen shows the patient claiming status (such as MEDICARE_PENDED or ASSESSED) when a Patient Claiming transaction is selected. |
67068 |
|
Transaction History (F8) Search for Batch |
Searching for data from the Transactions screen (F8) now included the following options: 1. Search for transactions by Batch Number. A search for batch number must provide a Provider name and batch Date, because batch numbers regenerate for each provider daily. 2. Search for transactions by Correlation ID. The Correlation ID is a unique identifier for a Medicare Web Services transaction. Operators may need to search for this ID in the transaction history for reconciliation purposes. |
68124 |
Bug Fixes
|
Function |
Release Notes |
Key |
|---|---|---|
|
MyComms |
When a new MyComms status is added, Bp VIP.net no longer updates the status of existing correspondence with a blank status. |
|
|
Patient Details |
You can no longer record dates of birth in the future in Patient Details. |
26003 |
|
Quotes |
Quote PDF files are now saved as 'Quote.pdf'' when attached to an email in Bp VIP.net, not Invoice.pdf. |
26091 |
|
DVA |
When billing DVA, all medical practitioners are now correctly paid 100% of the MBS fee for diagnostic imaging and pathology services. |
65263 |
|
In-Hospital Claims |
The value for Single Value Benefits (SVB) Number of Days is now submitted correctly for IHCW claims. |
68825 |
|
Multi-location and MWS |
The PRODA Login dialog that appears for practices with multiple Minor IDs now displays 'No B2B devices are near expiry' if no future expiry is detected, rather than appear blank. |
68598 |
|
Bulk reminders |
Duplicate profiles with the same name can no longer be saved in the Bulk Appointment Reminders screen. |
61589 |
|
Invoices |
When creating an invoice for Medicare or DVA, where one diagnostic imaging item number has been added that is not marked as self deemed and all remaining items are non referred items, the referral type is now set to 'D'. |
67677 |
|
Invoices |
When creating an invoice, service type defaults based on item type have been removed for all MBS items except Pathology items. You can set the service type from the Consultation (F5) screen. |
67605 |
|
Invoices |
Invoice items for anaesthesia claims now order correctly in F5. |
67536 |
|
Invoices |
When creating an invoice with multiple items, including a diagnostic imaging item, the referral Type Code and referral Override Code are now set correctly based on the presence of a referral and whether items are marked 'self-deemed'. |
67510 |
|
Claims |
For Australian practices, the Aus Claim Form (Alt+F8) screen now prompts that a Provider must be selected if this field is empty. |
67283 |
|
Patient Details |
White space padding in patient address details is truncated when the patient details are saved. This helps prevents batch errors related to address validation. |
67492 |
|
Payment F6 |
Tagging an invoice with no subsidiser and selecting the Medicare button no longer produces an error. |
68044 |
|
Tasks |
Cancelling a task reply no longer displays the task as 'Replied'. |
67802 |
|
My Health Record |
The text used in Bp VIP.net to indicate whether a patient has declined to upload all documents by default to My Health Record has been updated in accordance with Australia Digital Health Agency standards. |
64620 |
|
Patient Details |
Default cursor placement to the search box and tabbing order have been restored when adding a provider from the Patient Details (F3) screen. |
66811 |
|
IMC Claim Reporting |
The Total Benefit and HF BenefitAmount displayed on the IMC Claiming Payment report did not match the HF DepositAmount. This has been resolved and all totals match correctly. |
69119 |
Known Issues
|
Function |
Release Notes |
Key |
|---|---|---|
|
Patient Claiming |
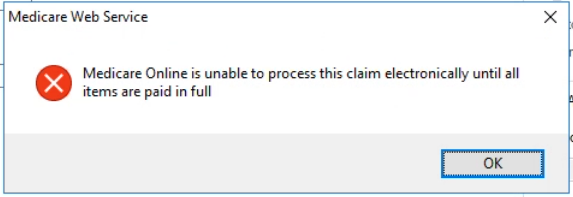
When sending a patient claim (PCI) for multiple items, Bp VIP.net cannot submit an invoice where a payment in the Payment screen (F6) exceeds the amount of the most expensive item, but is less than the total value of the whole invoice. Bp VIP.net will respond with the following alert.
For example, this scenario could occur when a patient is making a partial payment at the time, with the intention to complete the payment at a later date. Claims with multiple items must be paid or partially paid as follows to be successfully processed by Medicare:
Best Practice Software are working on a resolution in a future revision of Topaz SP1 to prevent this scenario occurring. Workaround Process the claim using one of these options:
The practice should aware that both workaround methods will invoke the Pay Doctor Via Claimant scheme, in which a cheque for the payment to doctor is issued by Medicare to the patient, who has 90 days to forward the cheque to the practice. Learn more about the Pay Doctor Via Claimant scheme. |
69062 |
|
Subsidiser Batching |
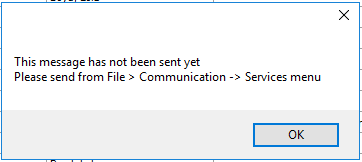
Batches cannot be resent from File > Communications > Subsidiser Batching by ticking Resend?. Bp VIP.net will respond with the following alert.
Workaround 1. Open the Transactions F8 screen of the billed organisation. 2. Select the batch to be resent. 3. Select Modify and Decline each item in the batch. 4. Modify each declined invoice from the patient's Transactions F8 screen and update the value in the Notes drop-down to Resubmission. Once all declined invoices have been modified and the Notes drop-down has been updated to Resubmission: 5. Select the Medicare icon. 6. Click option 4. Create & Send Batches. 7. Select Batch and Create / Send Batches to batch the resubmitted invoices and send. |
69139 |
|
Patient Claims Report |
The Patient Claims report does not show Rejected claims with (REJECTED) marker in Claim Type column when filtering the report for All. The report must be filtered for Rejected Only to show rejected claims with (REJECTED) marker in Claim Type column. This can be cross-referenced with the report for All . |
69121 |
|
Financial Summary |
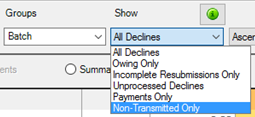
Filters in the Financial Summary using the Groups option for Batch results may include batches without the matching filter in the Show drop-down selection.
|
69082 |
|
Online Eligibility Check |
When running an OEC, the Online Eligibility Check (OECW) Report previewed in the Report Viewer screen will only save to the patient's MyComms F4 Incoming Correspondence if the Close button is selected. If any other option is used, the report will save as a blank PDF viewable from the Medicare button option 8. Online Eligibility Check Reporting, and will not save to the patient’s Incoming Correspondence.
|
69158 |
|
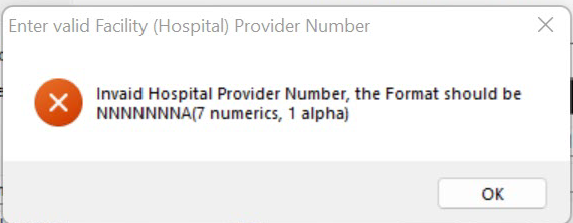
Medicare Web Services |
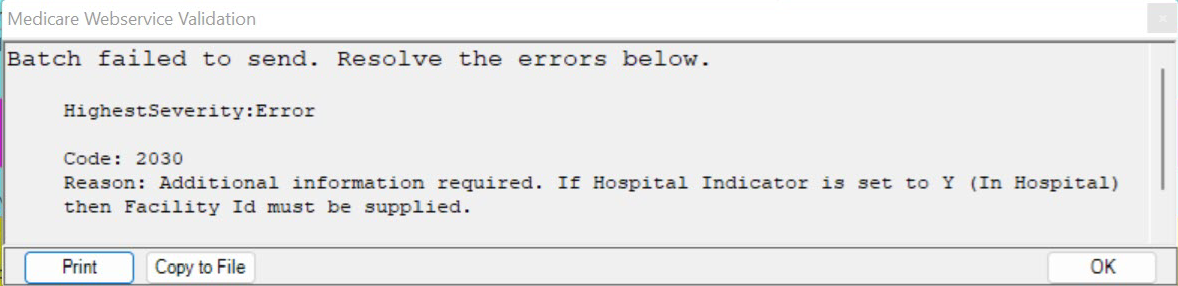
When creating a Bulk Billing batch for In-Patient claims, the Facility ID for the billing provider is populated incorrectly instead of the Facility ID of the hospital specified on the invoice. Users may not be able to create Bulk Billing batches if the Internal Facility in Bp VIP.net has no defined Facility ID or if the incorrect Facility ID is being included in the batch.
Workaround Users will need to create a matching provider record for the facility at which the operation was performed. Bp VIP.net will then populate the correct Facility ID from the provider record. If all existing internal providers already have an additional record at the hospital facility for billing purposes, continue to create these billing location records for all new providers. 1. Go to Setup > Providers > This Clinic 2. Select Copy Provider 3. The Unit will be the hospital that the operation was performed. If the hospital facility does not have an Internal Organisation record one must be created. 4. Select OK to save 5. Update the Provider details on the relevant invoices. |
69106 |
|
Medicare Web Services |
The interface to enable Medicare Web Services may not be visible to users after 1 July 2022. Contact Bp VIP.net support to have a script run to enable Medicare Web Services. |
69250 |