In-patient Medical (IMC) and In-hospital Medical (IHC) claims reports are available in Bp VIP.net Australia for analysing unprocessed, processed (paid), and declined IMC and IHC claims and manual reconciliation of payments.
The examples in this article use IMC reports to demonstrate, but the screens for generating IHC reports are the same. IHC reports contain similar information but often with more detail on services, given the nature of in-hospital consultations.
In this article:
- View IMC and IHC claims and run a report
- Processing reports
- Payment reports
- Paid and Processing reports
- All reports
- Declined reports
- Checking the patient contribution for IMC and IHC Claims
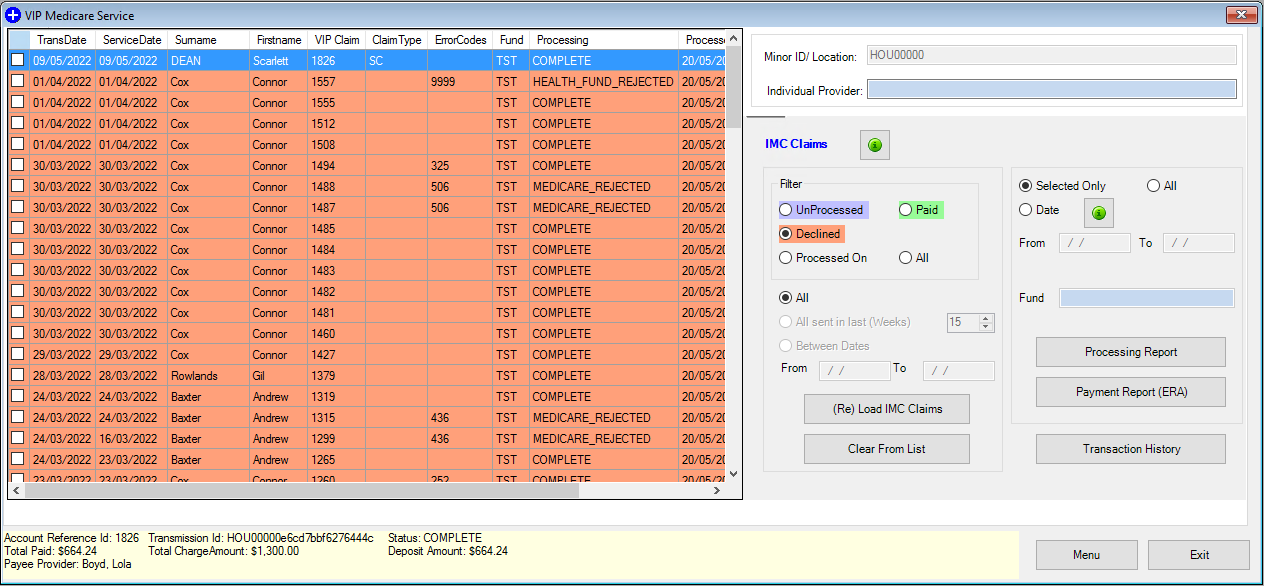
View IMC and IHC claims and run a report
- Select the Medicare icon from the toolbar.
- If your practice has multiple Locations and Minor IDs that require multiple B2B registrations, select the Location and B2B device to report on.
- Select 2. IMC Claim Reporting or 9. IHC Claim Reporting. The VIP Medicare Service scree will open.
- The Minor ID/Location field displays the location you are reporting on and cannot be changed. You can select an Individual Provider if you wish to filter reports to a single provider.
- From the left hand panel, select the types of claims to view from the Filter options, such as Paid or Declined. The options are described in this article.
- Select a date range to return claims for: All claims, All sent in last n weeks, or supply a From and To date range.
- Click Load IMC / IHC Claims.
View claims
- From the right hand panel, click Selected Only if you are running a report only on claims that you have ticked from the returned list. Otherwise, tick All.
- Specify a Date range of up to 31 days to include in the report.
- If you specify a date range, you can also nominate a single Fund (insurers only) to filter the report on.
- Click Payment Report or Process Report to generate the report.
Print a report
Processing reports
The processing report shows each transmitted claim, showing patient details, fund details, and each item’s benefit details. The Status of a report in the upper right shows the status for the submitted batch and can be one of:
- COMPLETE
- MEDICARE_REJECTED
- HEALTH_FUND_REJECTED.
The Service Fund Assessment Code column provides the acceptance status of individual claims.
The Account Reference Id in the top left is the number needed when enquiring for any further information on the claim from the health fund or Medicare. The Reason Code Explanation list at the bottom of the report explains the Explanation Code columns and supplies any reasons for rejection.
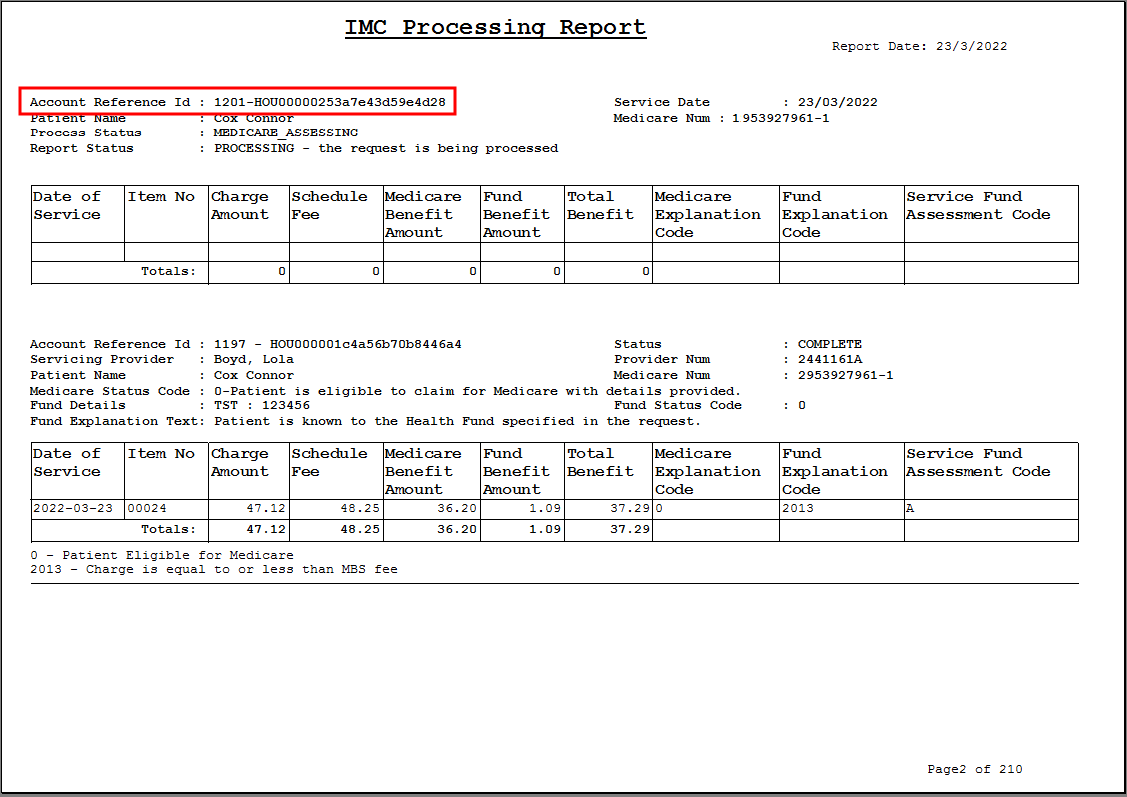
The process report lets you know that you are going to receive a payment, but does not specify when. Actual payment information is supplied in the payment report.
Payment reports
The payment report occurs only when amounts are deposited into your bank account. The report shows transaction details for all payments attached to a claim. Details are not included for unpaid claims.
The PaymentRunDate indicates the date on which the money was deposited into the bank account. The Payment Reference indicates the reference against the payment from the organisation's transaction history (F8).
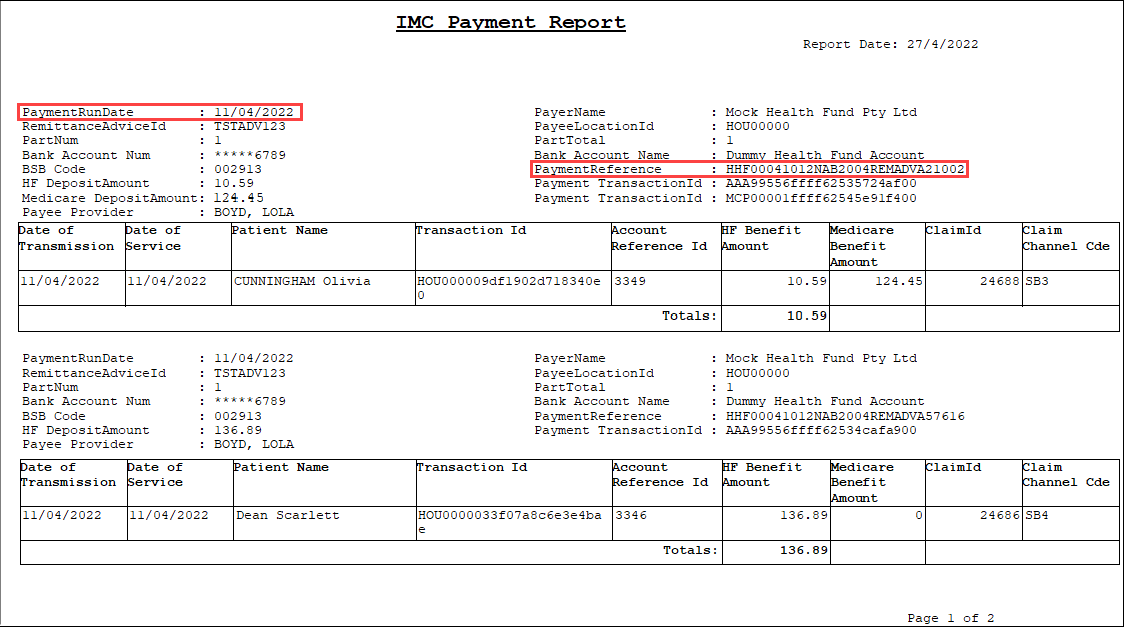
You should call Medicare or the health fund if you have not received an expected payment within 14 days.
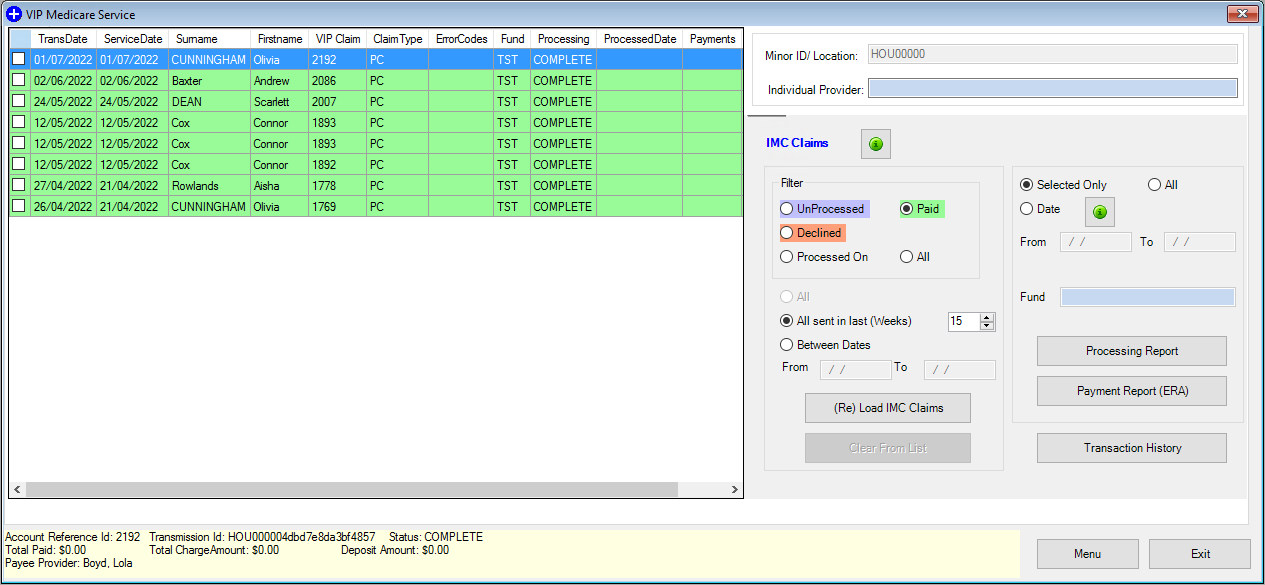
Paid and Processing reports
Select the type of report you want to see from the Filter radio buttons on the right.
The Paid report shows which patients have been paid between any selected date period, as long as the payment is within six months of transmitting.
The Processed report breaks down each payment made into the account by date, patient, item and amount.
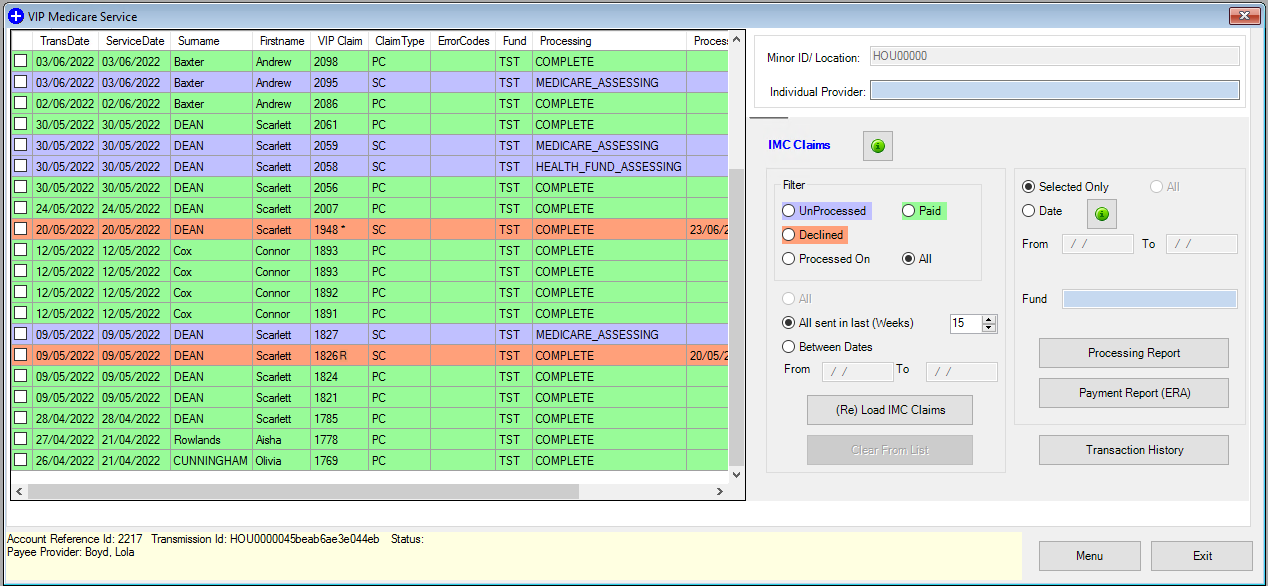
All reports
When selecting the All report, choose the date range for the transactions you would like to see. The report will show the following claims:
- Unprocessed
- Paid
- Overpayment included (dark green)
- Declined.
An asterisk (*) is visible in the VIP Claim column if the claim was cleared from the list manually. The letter 'R' will be visible in the VIP Claim column if the claim was resubmitted.
Declined reports
The Declined report shows which claims have been declined by the health fund or Medicare and why. This report also includes claims that are paid less than the charge amount. You can resubmit any claim if the claim was paid less than the charge amount or rejected for any reason, after the account has been corrected.
Select the green information icon at the top right of the IMC Claims panel to view some of the most common reject code explanations.
See Resubmit a declined IMC Claim for more information.
NOTE There is no facility to delete a claim once accepted by the ECLIPSE hub. If you need to delete a claim after this time, contact the helpdesk
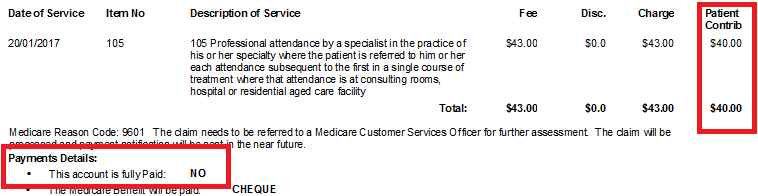
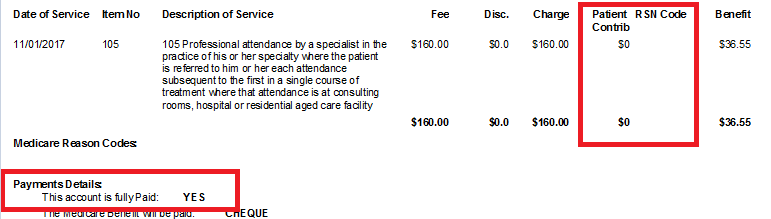
Checking the patient contribution for IMC and IHC Claims
When a claim is sent to Medicare, the patient contribution is shown in the claims reports if the patient makes a payment towards the owing account.
If a patient pays only a portion of the account, in the Payments Details section 'This account is fully paid: NO' will be shown. The actual contribution paid is shown under the Patient Contribution column.
If the patient pays the full amount owed, the patient contribution will show as $0 and the Payment Details will state 'This account has been fully Paid: YES'.
Related topics
Last modified: 11 August 2022