You can process Bulk Bill, DVA, and Patient claims in Bp Allied using Medicare Online Claiming.
On this page
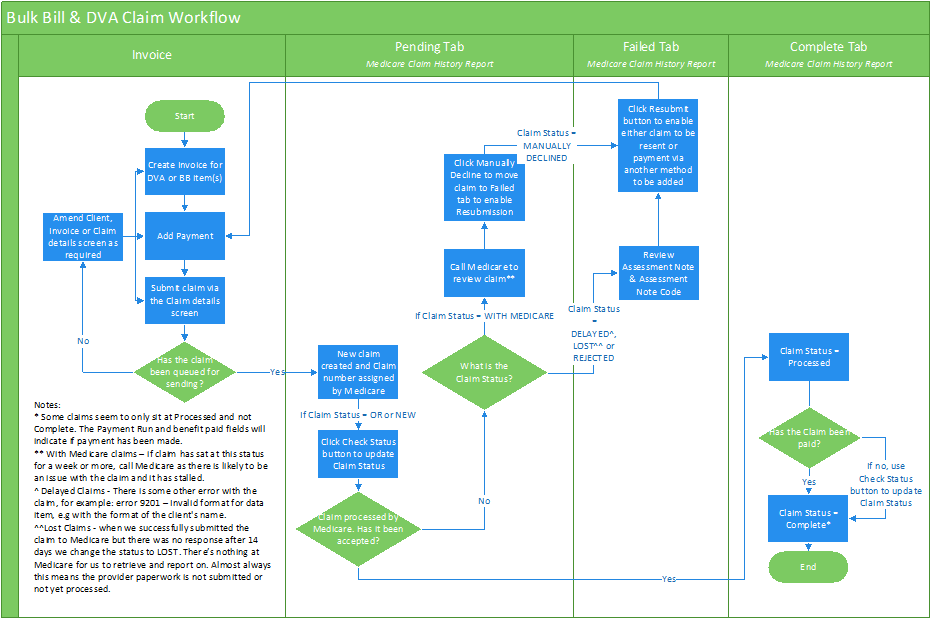
Bulk Bill & DVA Claims
Creating Claims
Bulk Bill and DVA Claims are created when an Invoice payment is made.
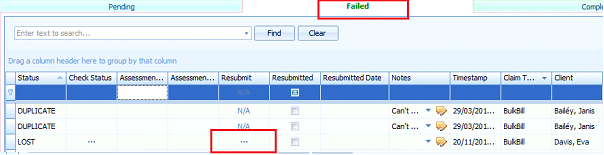
Resubmitting Claims
Bulk Bill and DVA Claims are resubmitted from the Medicare Claim History Report.
- Navigate to Reports from the left-hand menu.
- Under Medicare, select Medicare Claim History Report.
- Select the Failed tab of the report.
- Select the ellipsis [...] icon in the Resubmit column.
- Use the Assessment Code and Assessment Code Note along with the information from Medicare and DVA to ascertain why a claim has been rejected.
Medicare and DVA troubleshooting resources can be found in the following links:
- Medicare reason codes and reducing claim rejections
- Medicare digital claiming return codes
- DVA reason codes
Patient Claims
Creating Claims
Patient claims are managed differently to Bulk Bill & DVA claims due to the way the payment for services is received Full payment from the patient is received when creating patient claims, and the Medicare rebate is not received by the practice.
Details from Medicare such as payment status can not be viewed in Bp Allied. A Patient Claim cannot have a Claim Status of Processed or Complete in Bp Allied, all Patient claims are located in the Pending tab.
Patient Claims have a Claim Type of Medicare.
Resubmitting Claims
- From the Medicare Claim History Report select the In Progress tab.
- Select the ellipses [...] in the Manual Decline column.
- Enter the relevant details from the information received from the patient.
- Select the Failed tab to locate the claim
- Select the ellipsis [...] icon in the Resubmit column.
- Use the Assessment Code and Assessment Code Note along with the information from Medicare and DVA to ascertain why a claim has been rejected.
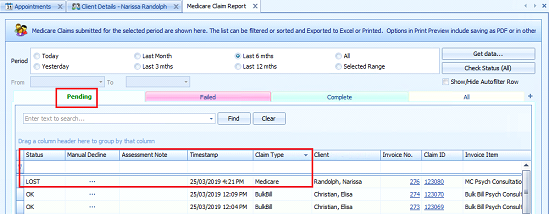
A status of With Medicare, Delayed or Lostmay be returned if a review of the details submitted with the claim is required. These patient claims can be viewed in the Pending tab.
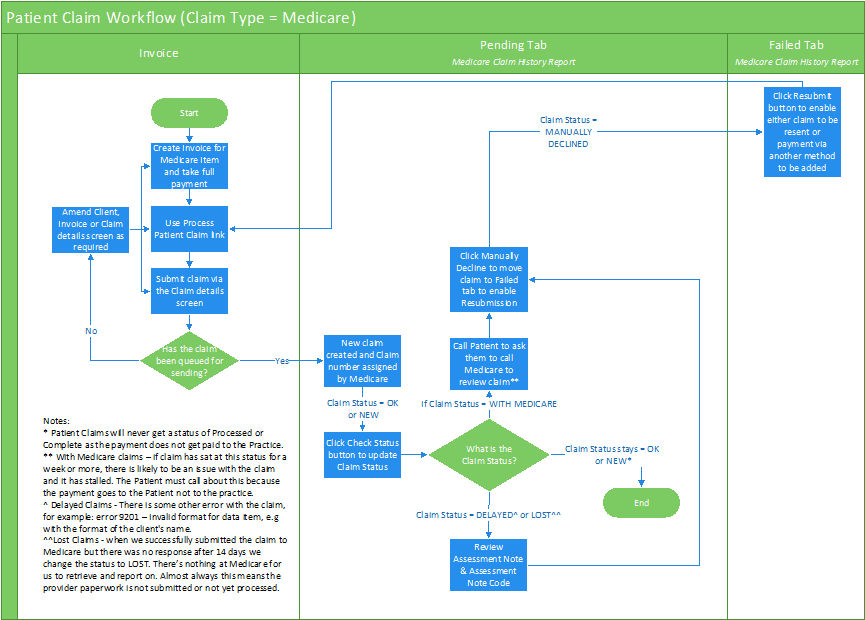
See Manually Decline a Claim for further information.
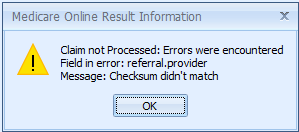
Claim Processing Errors
When an error is returned from Medicare a message will display in the following format:
-
Field in error: displays the tab and field where the error has occurred in the format of 'tabname.fieldname'.
-
Message: displays the error with the field.
Potential errors when processing a claim
|
Field in Error |
Error message |
What this means |
|---|---|---|
|
referral.provider |
Checksum didn't match |
In the Referral tab, the Provider Number is not correct. |
|
referral.date |
Must be after [patient.dateofbirth] and be before today and be before [item.date] |
In the Referral tab, the referral date field is at a future time. It should be a date between the patients DOB and the date of the appointment. Both of these dates must be before today's date. |
|
provider.servicing |
Checksum didn't match |
In the Provider tab, the Practitioners (servicing) Provider Number is not correct. |
|
patient.medicare.number |
Medicare Card Number should be 11 characters long. |
In the Patient tab, the Medicare Card Number is missing or incomplete. |
|
patient.medicare.number |
Checksum didn't match |
In the Patient tab, the Medicare Card Number is not a valid number. |
|
patient.medicare.ref |
Invalid data type. Should be an unsigned integer. |
In the Patient tab, the Medicare Card Reference is missing or incomplete. |
|
patient.dateOfBirth |
Expected string containing date (YYYY-MM-DD) |
In the Patient tab, the date of birth field has a problem. Either the date is a future date or it is too far into the past. |
|
flags.account paid |
Required |
In the Flags tab, the Account Paid field is not ticked. This is required before a Patient claim can be processed. |