Day stay episodes can be charged in one or a combination of three ways, depending on the contract your hospital has with each health fund.
- DRG - Some contracts with health funds will base fees on DRG codes. DRG codes are generated from the Discharge Summary screen based on the procedural and diagnostic codes associated with the stay. These incorporate both the theatre and accommodation fees. Some prostheses can be included as part of the DRG item fee, depending on individual contracts your clinic has with the health fund.
- Case Based - Each procedural item code has a case base fee and a procedure fee. Depending on the contract:
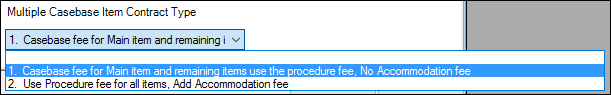
- Some contracts use the case base fee for the item with the highest theatre band for multiple procedure operations and subsequent items are charged on the procedure fee. Accommodation is not charged.
- Other contracts charge each item as the procedure fee and an Accommodation fee is charged.
- Per diem - The patient is charged the accumulation of theatre and accommodation costs. Theatre bands are derived from MBS item codes. Theatre band charges and accommodation charges for top cover are set according to individual contracts your clinic has with the health fund. If a patient has base medical cover then base cover accommodation rates are charged. Although many theatre band charges can be used in a multiple procedure operation, only one accommodation fee can be charged. The items will be charged in the order of the highest theatre band.
Some prostheses can be included in the case base item fee depending on individual contracts your clinic has with the health fund. The items will be charged in the order of the highest procedure cost.
NOTE If the prosthesis model used is not a prosthesis included in the DRG or case base fee, the different prosthesis needs to be added to the Operation screen or Day Stay Episode as a separate item prior to generating the Invoice.
For each Day Stay Episode generated in Bp VIP.net, accommodation bands are calculated using the anaesthetic type and the theatre time duration from the Discharge Details screen.
In addition, for operations with multiple procedures, insurers will also stipulate a percentage of cover for the most expensive procedure and decrease the cover for subsequent procedures in the same day stay episode. Normally, cover will be 100% for the most expensive procedure’s fee, but this is contract dependent.
At invoice generation during discharge, Bp VIP.net will determine the billing method from the Health Fund Contracts tab of the patient’s health fund’s organisation details. For multiple procedure operations, Bp VIP.net will bill fees in the following order; DRG charges first, if any are present, then case based charges if any are present and finally, any per diem fees.
DRG, case base or per diem invoicing
The rules applied to the items in the invoice depends on the how the chargeable items are set up in the Health Fund Contract tab of the health fund details.
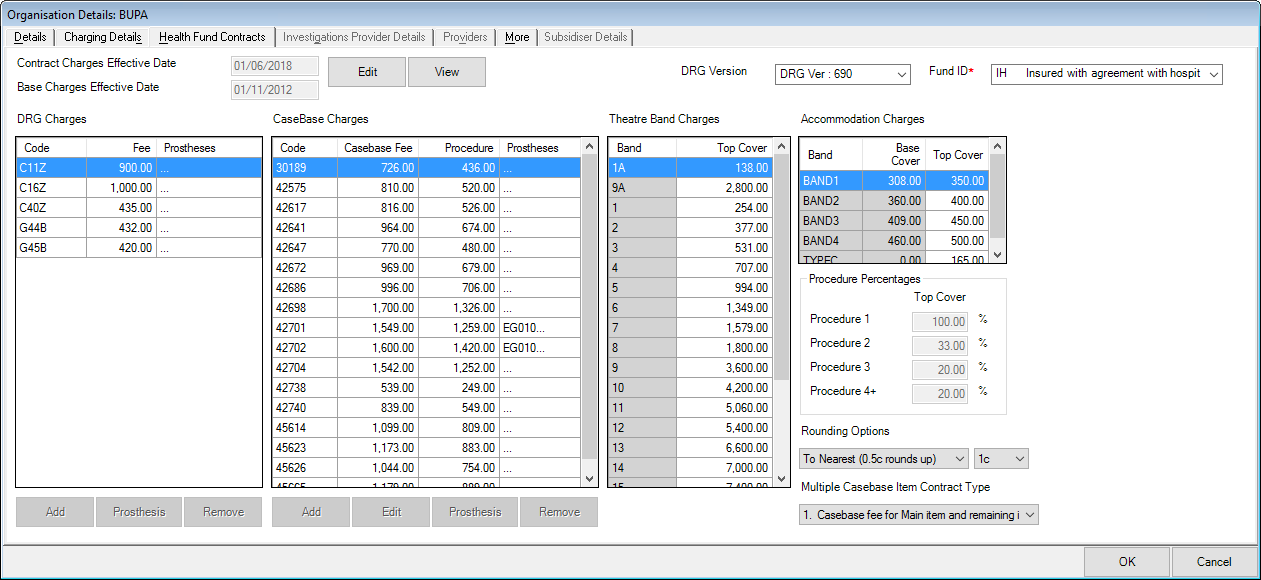
The example above shows four main columns:
- The DRG Charges
- The Case Base Charges
- Theatre Band Charges
- Accommodation Charges
DRG Billing
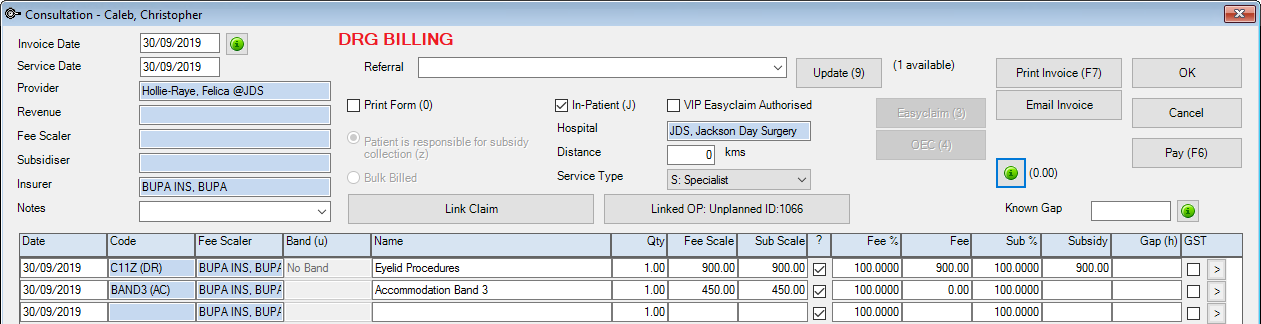
When the Diagnoses tab of the Day Stay Episode is completed, an appropriate DRG code must be generated by clicking the Generate DRG button for reporting purposes.
If the generated DRG code matches the health fund’s contracted DRG code, the DRG item code will be populated into the invoice.
IMPORTANT If the DRG code 960Z Ungroupable is selected in the Diagnoses and Procedures tab of the Day Stay Episode, then the billing will default to case base or per diem.
As the patient above had a procedure that was grouped into the DRG code of C11Z and their health fund has a contract that includes the DRG code, the item billed is the DRG code contract charge.
Although the Accommodation Band 3 has been generated from the Day Stay Episode, the accommodation cost is included as part of the DRG item fee and is not charged as an extra item but displayed for the health fund.
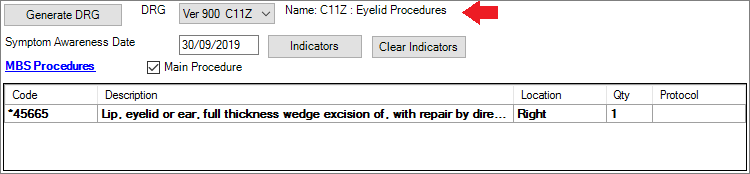
Case base billing
The two items (42702 and 42738) were added to the patient’s operation screen and subsequently populated into the Day Stay Episode. They are both case base charges under the patient’s health fund. As 42702 is the more expensive item with a higher theatre band, the case base fee will apply.
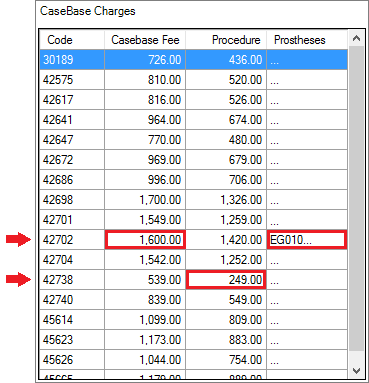
Because the health fund has both items in their contract, both items are charged as case base (CB).
- Theatre Band is not displayed as this item is case base.
- The 2nd item is charged the procedure fee due to the rule selected in the Multiple Casebase Item Contract Type in the health fund. This will be the less expensive item.
- There is no item charge for the prosthesis as this is included in the health fund contract for item 42702. If a prosthesis is not included in the health fund contract for a procedure item, the invoice will display it as an additional charged item.
- The Accommodation Band has been generated into the invoice but the patient is not charged individually for this as it is included in the case base fee for the main procedure.
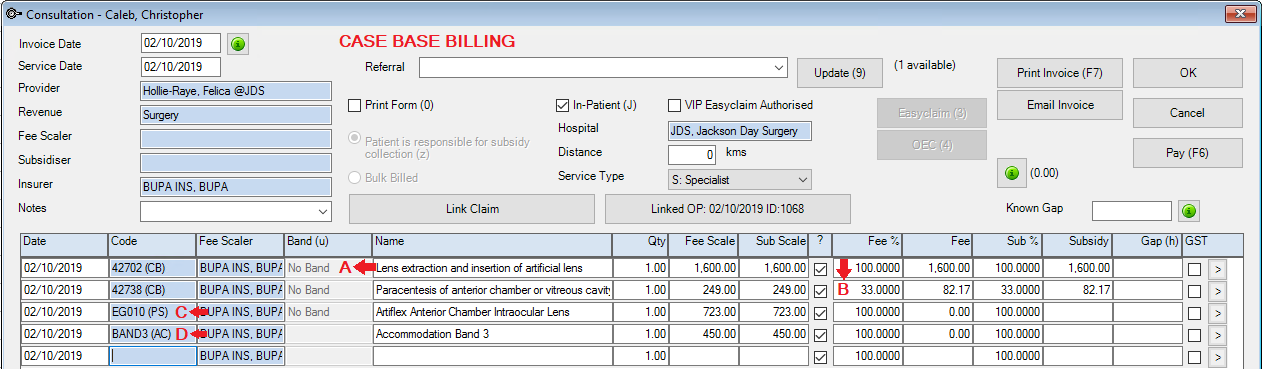
Per diem billing
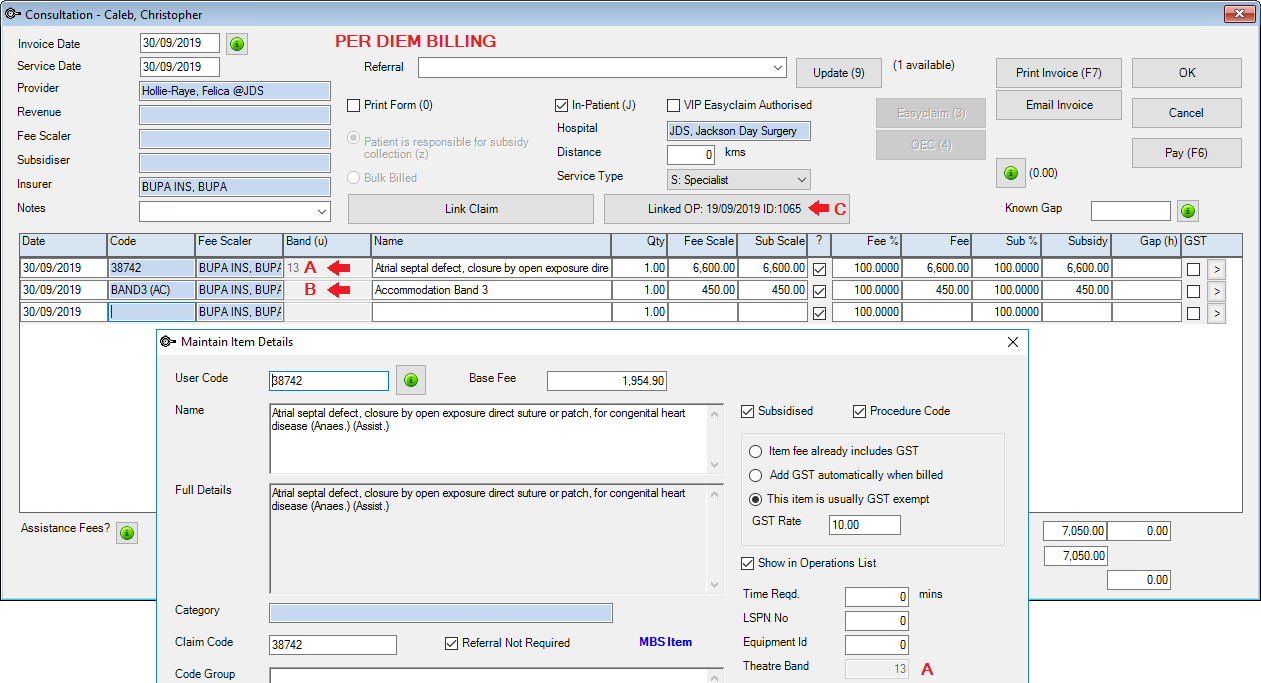
If the procedure item is not on the health fund contract as a DRG or case based, the day stay invoice will display a combination of the accommodation charges and the theatre band charges.
- The Theatre Band is populated from the Item – this is set by MBS
- The Accommodation Band is generated and populated from the Day Stay Episode.
- The day stay invoice will be linked to the operation booking.
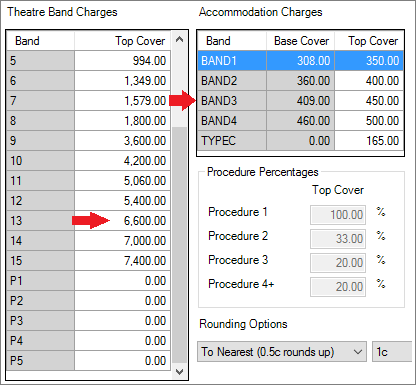
- If there are multiple procedure items on the day stay invoice, then the procedure percentages will apply, and the most expensive item will be charged as procedure 1.
- There can only be one charged accommodation band on the day stay invoice.
- If the patient has top cover recorded on their Patient Details, they will be charged top cover. If the patient has base cover recorded, they will be charged will base cover for the accommodation charge.
Last modified: July 2020